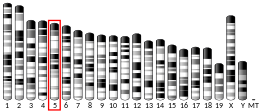
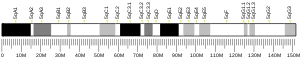
Toll-like receptor 1 (TLR1) is a member of Toll-like receptors (TLRs), which is a family of pattern recognition receptors (PRRs) that form the cornerstone of the innate immune system.[5][6][7] TLR1 recognizes bacterial lipoproteins and glycolipids in complex with TLR2. TLR1 is a cell surface receptor.[5] TLR1 is in humans encoded by the TLR1 gene, which is located on chromosome 4.[8]
Function
editThe binding of ligands to TLR1 activates intracellular signaling cascades leading to an inflammatory response and initiation of immune processes.[5][9]
TLR1 cooperates with TLR2 in the recognition of bacterial triacyl lipoproteins. TLR1 has been shown to recognize the outer surface lipoprotein of Borrelia burgdorferi. The important role of TLR1 in recognizing triacyl lipopeptides has been shown in TLR1-deficient mice.[9][10]
Toll-like receptors, including TLR-1, found on the epithelial cell layer that lines the small and large intestine are important players in the management of the gut microbiota and detection of pathogens.[11]
Expression
editTLR1 is synthesized in the endoplasmic reticulum. The trafficking of TLR1 from endoplasmic reticulum is controlled by protein associated with TLR4 (PRAT4A), which is endoplasmic reticulum resident chaperone. TLR1 is then transported to Golgi complex and to cell membrane.[12]
TLR1 mRNA was expressed at high levels in the kidney, lung, and spleen in adult humans, but in low levels in fetal brain and liver as well as in HeLa cell line.[13]
TLR1 is expressed in the highest levels on NK cells compared to other TLRs. TLR1 has been found to be expressed on human peripheral blood γδT cells, myeloid-derived suppressor cells, platelets, CD4+ T cells, microglia, astrocytes, immature dendritic cells, LTi-like innate lymphoid cells[12] and eosinophils.[14] It is also found on the surface of macrophages and neutrophils.[citation needed]
Structure
editTLR1 is a type I transmembrane glycoprotein composed of extracellular, transmembrane and intracellular domains.[5]
The extracellular domain of TLR1 contains leucine-rich repeat (LRR) domains, which play a crucial role in binding PAMPs. The LRR domains can be further categorized into three subdomains: the N-terminal, central, and C-terminal regions. While the N-terminal and C-terminal domains of TLR1 exhibit relative consistency with a consensus amino acid structure represented as xLxxLxxLxLxxNxLxxLPxxxFx, the central domains display significant variability. Notably, the central domains of TLR1 lack the presence of stabilizing asparagine ladders, which contribute to the typical horseshoe-like shape of the extracellular domain of TLRs. Furthermore, the number of residues within the LRR domains of the central region varies between 20 and 33 residues. Additionally, extra alpha helices were found in central domains of TLR1. The biological function of TLR1 is closely linked to the structural modifications in its extracellular domain, which are responsible for its capacity to bind ligands.[15]
The intracellular domain of TLR1 consists of a Toll/interleukin-1 receptor (TIR) domain, which is shared by various adaptor proteins involved in the signaling cascade initiated by TLRs. The TIR domain of TLR1 has been found as a monomer in the crystal structure.[16]
TLR1 is able to recognize ligands as a complex with TLR2, referred to as TLR2/1 heterodimer. TLR2 can heterodimerize also with TLR6 forming TLR2/6 heterodimer. TLR2/1 adopts an "m"-shaped conformation when interacted with its ligands. The "m" shape conformation is formed by extracellular domains of TLR1 and TLR2, bringing the transmembrane and intracellular domains in close association. This conformational arrangement subsequently triggers a downstream signaling cascade.[16][17]
TLR2/1 specifically recognizes triacyl lipopeptides, whereas TLR2/6 recognizes diacyl lipopeptides. Diacyl and triacyl lipopeptides are present on the bacterial outer membrane. In the case of triacyl lipopeptides, the mechanism behind their recognition lies in the incorporation of two lipid chains into the hydrophobic pocket of TLR2, while the remaining lipid chain inserts into a hydrophobic pocket of TLR1. Regarding TLR6, the hydrophobic pocket is obstructed by the side chains of two phenylalanine residues, resulting in a smaller pocket than in TLR1. This structural difference accounts for the distinct ligand specificities exhibited by TLR2/1 and TLR2/6 heterodimers.[17]
Interactions
editTLR1 has been shown to interact with TLR2.[18] TLR1 recognizes peptidoglycan and (triacyl) lipopeptides in concert with TLR2 (as a heterodimer).[19][20]
References
edit- ^ a b c GRCh38: Ensembl release 89: ENSG00000174125 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000044827 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b c d El-Zayat SR, Sibaii H, Mannaa FA (2019-12-12). "Toll-like receptors activation, signaling, and targeting: an overview". Bulletin of the National Research Centre. 43 (1): 187. doi:10.1186/s42269-019-0227-2. ISSN 2522-8307. S2CID 257116233. This article incorporates text from this source, which is available under the CC BY 4.0 license.
- ^ Rock FL, Hardiman G, Timans JC, Kastelein RA, Bazan JF (January 1998). "A family of human receptors structurally related to Drosophila Toll". Proceedings of the National Academy of Sciences of the United States of America. 95 (2): 588–593. Bibcode:1998PNAS...95..588R. doi:10.1073/pnas.95.2.588. PMC 18464. PMID 9435236.
- ^ Lien E, Ingalls RR (January 2002). "Toll-like receptors". Critical Care Medicine. 30 (1 Suppl): S1-11. doi:10.1097/00003246-200201001-00001. PMID 11782555.
- ^ "UniProt". www.uniprot.org. Retrieved 2023-06-18.
- ^ a b Takeda K, Kaisho T, Akira S (2003). "Toll-like receptors". Annual Review of Immunology. 21: 335–376. doi:10.1146/annurev.immunol.21.120601.141126. PMID 12524386.
- ^ Takeda K, Akira S (April 2015). "Toll-like receptors". Current Protocols in Immunology. 109 (1): 14.12.1–14.12.10. doi:10.1002/0471142735.im1412s109. PMID 25845562. S2CID 44291946.
- ^ de Kivit S, Tobin MC, Forsyth CB, Keshavarzian A, Landay AL (2014). "Regulation of Intestinal Immune Responses through TLR Activation: Implications for Pro- and Prebiotics". Frontiers in Immunology. 5: 60. doi:10.3389/fimmu.2014.00060. PMC 3927311. PMID 24600450.
- ^ a b Vijay K (June 2018). "Toll-like receptors in immunity and inflammatory diseases: Past, present, and future". International Immunopharmacology. 59: 391–412. doi:10.1016/j.intimp.2018.03.002. PMC 7106078. PMID 29730580.
- ^ Nishimura M, Naito S (May 2005). "Tissue-specific mRNA expression profiles of human toll-like receptors and related genes". Biological & Pharmaceutical Bulletin. 28 (5): 886–892. doi:10.1248/bpb.28.886. PMID 15863899.
- ^ Kvarnhammar AM, Cardell LO (May 2012). "Pattern-recognition receptors in human eosinophils". Immunology. 136 (1): 11–20. doi:10.1111/j.1365-2567.2012.03556.x. PMC 3372752. PMID 22242941.
- ^ Jin MS, Lee JO (August 2008). "Structures of the toll-like receptor family and its ligand complexes". Immunity. 29 (2): 182–191. doi:10.1016/j.immuni.2008.07.007. PMID 18701082.
- ^ a b Botos I, Segal DM, Davies DR (April 2011). "The structural biology of Toll-like receptors". Structure. 19 (4): 447–459. doi:10.1016/j.str.2011.02.004. PMC 3075535. PMID 21481769.
- ^ a b Kaur A, Kaushik D, Piplani S, Mehta SK, Petrovsky N, Salunke DB (January 2021). "TLR2 Agonistic Small Molecules: Detailed Structure-Activity Relationship, Applications, and Future Prospects". Journal of Medicinal Chemistry. 64 (1): 233–278. doi:10.1021/acs.jmedchem.0c01627. PMID 33346636. S2CID 229341059.
- ^ Takeuchi O, Sato S, Horiuchi T, Hoshino K, Takeda K, Dong Z, et al. (July 2002). "Cutting edge: role of Toll-like receptor 1 in mediating immune response to microbial lipoproteins". Journal of Immunology. 169 (1): 10–14. doi:10.4049/jimmunol.169.1.10. PMID 12077222.
- ^ Farhat K, Riekenberg S, Heine H, Debarry J, Lang R, Mages J, et al. (March 2008). "Heterodimerization of TLR2 with TLR1 or TLR6 expands the ligand spectrum but does not lead to differential signaling". Journal of Leukocyte Biology. 83 (3): 692–701. doi:10.1189/jlb.0807586. PMID 18056480. S2CID 1129471.
- ^ Jin MS, Kim SE, Heo JY, Lee ME, Kim HM, Paik SG, et al. (September 2007). "Crystal structure of the TLR1-TLR2 heterodimer induced by binding of a tri-acylated lipopeptide". Cell. 130 (6): 1071–1082. doi:10.1016/j.cell.2007.09.008. PMID 17889651. S2CID 10992433.
External links
edit- Toll-Like+Receptor+1 at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- PDBe-KB provides an overview of all the structure information available in the PDB for Human Toll-like receptor 1 (TLR1)
This article incorporates text from the United States National Library of Medicine ([1]), which is in the public domain.