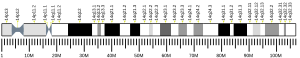
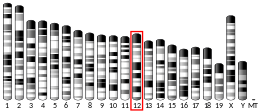
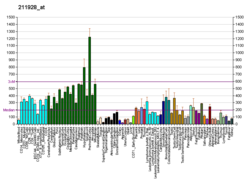
Cytoplasmic dynein 1 heavy chain 1 is a protein that in humans is encoded by the DYNC1H1 gene.[5][6][7] Dynein is a molecular motor protein that is responsible for the transport of numerous cellular cargoes to minus ends of microtubules, which are typically found in the center of a cell, or the cell body of neurons. It is located on the 14th chromosome at position 14q32.31.[5] Cytoplasmic dynein transports cargoes along the axon in the retrograde direction, bringing materials from the axon to the cell body. Dynein heavy chain binds microtubules and hydrolyzes ATP at its C-terminal head.[8] It binds cargo via interaction with other dynein subunits at its N-terminal tail.[9]
Interactions
editDYNC1H1 has been shown to interact with a large variety of proteins that act as adaptors and regulators. The dynein motor protein complex itself is a large, 1.4 MDa multimeric complex composed of dimerized heavy chains, two intermediate chains, two light intermediate chains, and additional light chains.[8] Other well known adaptors and regulators are Dynactin, PAFAH1B1[10] and CDC5L.[11]
Clinical relevance
editDefects in axonal transport, of which dynein plays a key role, have been implicated in conditions ranging from developmental defects in the brain to neurodegenerative disease.[9] Mutations in the DYNC1H1 gene have been associated with epilepsy, neuromuscular disease, brain malformations, intellectual disability, autism, and neurodegenerative diseases.[12] These as a whole are considered to be DYNC1H1-Related Disorders[12] or dyneinopathies.[13] Recent data implies that DYNC1H1-Related Disorders should be considered progressive, though the trigger and symptoms of that progress vary from patient to patient.[12] As of September 1, 2024, nearly 1900 gene variants have been identified and classified as either pathogenic, likely pathogenic, or variants of unknown significance.[14] The vast majority of these are missense mutations. Due to a high degree of pleiotropy, the genotype-phenotype spectrum is still developing.[15] Given the heterogeneity of symptoms, large gene size, and the high conservation of the gene,[16] it is likely that many patients remain undiagnosed. In recent larger cohort studies, the average age of patients was only 12 years old, likely due to symptoms overlap with other disorders like cerebral palsy and idiopathic autism and intellectual disability.[12]
Prior to genetic testing, clinical diagnoses for these symptoms range from Charcot-Marie-Tooth disease[17] as well as spinal muscular atrophy with lower extremity predominance 1 (SMA-LED1).[18] Another symptom is Autosomal dominant non-syndromic intellectual disability.[19] DYNC1H1 gene variants have been increasingly correlated with Amyotrophic lateral sclerosis,[20][21] malformations of cortical development, and seizure disorders.[22] It is estimated that roughly 40% of patients with DYNC1H1 gene variants have epilepsy, and 80-92% of those with DYNC1H1-related epilepsy have malformations of cortical development, including both lissencephaly and polymicrogyria.[22][23]
Society and Culture
editThe DYNC1H1 Association (dync1h1.org), a non-profit patient advocacy organization, was founded in 2023 with the goal of accelerating research into treatments for DYNC1H1-related disorders. The three founders are parents of children who have DYNC1H1-related disorders.
References
edit- ^ a b c GRCh38: Ensembl release 89: ENSG00000197102 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000018707 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b Pfister KK, Fisher EM, Gibbons IR, Hays TS, Holzbaur EL, McIntosh JR, et al. (November 2005). "Cytoplasmic dynein nomenclature". J Cell Biol. 171 (3): 411–3. doi:10.1083/jcb.200508078. PMC 2171247. PMID 16260502.
- ^ Vaisberg EA, Grissom PM, McIntosh JR (August 1996). "Mammalian cells express three distinct dynein heavy chains that are localized to different cytoplasmic organelles". J Cell Biol. 133 (4): 831–42. doi:10.1083/jcb.133.4.831. PMC 2120833. PMID 8666668.
- ^ "Entrez Gene: DYNC1H1 dynein, cytoplasmic 1, heavy chain 1".
- ^ a b Berth SH, Lloyd TE (June 2023). "Disruption of axonal transport in neurodegeneration". The Journal of Clinical Investigation. 133 (11). doi:10.1172/JCI168554. PMC 10232001. PMID 37259916.
- ^ a b Cason SE, Holzbaur EL (November 2022). "Selective motor activation in organelle transport along axons". Nature Reviews. Molecular Cell Biology. 23 (11): 699–714. doi:10.1038/s41580-022-00491-w. PMID 35637414.
- ^ Tai CY, Dujardin DL, Faulkner NE, Vallee RB (March 2002). "Role of dynein, dynactin, and CLIP-170 interactions in LIS1 kinetochore function". The Journal of Cell Biology. 156 (6): 959–968. doi:10.1083/jcb.200109046. PMC 2173479. PMID 11889140.
- ^ Ajuh P, Kuster B, Panov K, Zomerdijk JC, Mann M, Lamond AI (December 2000). "Functional analysis of the human CDC5L complex and identification of its components by mass spectrometry". The EMBO Journal. 19 (23): 6569–6581. doi:10.1093/emboj/19.23.6569. PMC 305846. PMID 11101529.
- ^ a b c d Möller B, Becker LL, Saffari A, Afenjar A, Coci EG, Williamson R, et al. (June 2024). "The expanding clinical and genetic spectrum of DYNC1H1-related disorders". Brain. doi:10.1093/brain/awae183. PMID 38848546.
- ^ Marzo MG, Griswold JM, Ruff KM, Buchmeier RE, Fees CP, Markus SM (July 2019). "Molecular basis for dyneinopathies reveals insight into dynein regulation and dysfunction". eLife. 8: e47246. doi:10.7554/eLife.47246. PMC 6733598. PMID 31364990.
- ^ "DYNC1H1". ClinVar. U.S. National Library of Medicine. Retrieved 2024-10-03.
- ^ Li JT, Dong SQ, Zhu DQ, Yang WB, Qian T, Liu XN, et al. (2022-07-11). "Expanding the Phenotypic and Genetic Spectrum of Neuromuscular Diseases Caused by DYNC1H1 Mutations". Frontiers in Neurology. 13: 943324. doi:10.3389/fneur.2022.943324. PMC 9309508. PMID 35899263.
- ^ Cho C, Vale RD (January 2012). "The mechanism of dynein motility: insight from crystal structures of the motor domain". Biochimica et Biophysica Acta (BBA) - Molecular Cell Research. 1823 (1): 182–191. doi:10.1016/j.bbamcr.2011.10.009. PMC 3249483. PMID 22062687.
- ^ Weedon MN, Hastings R, Caswell R, Xie W, Paszkiewicz K, Antoniadi T, et al. (August 2011). "Exome sequencing identifies a DYNC1H1 mutation in a large pedigree with dominant axonal Charcot-Marie-Tooth disease". American Journal of Human Genetics. 89 (2): 308–312. doi:10.1016/j.ajhg.2011.07.002. PMC 3155164. PMID 21820100.
- ^ Harms MB, Ori-McKenney KM, Scoto M, Tuck EP, Bell S, Ma D, et al. (May 2012). "Mutations in the tail domain of DYNC1H1 cause dominant spinal muscular atrophy". Neurology. 78 (22): 1714–1720. doi:10.1212/WNL.0b013e3182556c05. PMC 3359582. PMID 22459677.
- ^ "Orphanet: Rare non-syndromic intellectual disability". www.orpha.net. Retrieved 2024-10-03.
- ^ Zhou Z, Kim J, Huang AY, Nolan M, Park J, Doan R, et al. (December 2023). "Somatic Mosaicism in Amyotrophic Lateral Sclerosis and Frontotemporal Dementia Reveals Widespread Degeneration from Focal Mutations". bioRxiv. doi:10.1101/2023.11.30.569436. PMC 10705414. PMID 38077003.
- ^ Mentis AA, Vlachakis D, Papakonstantinou E, Zaganas I, Patrinos GP, Chrousos GP, et al. (February 2022). "A novel variant in DYNC1H1 could contribute to human amyotrophic lateral sclerosis-frontotemporal dementia spectrum". Cold Spring Harbor Molecular Case Studies. 8 (2): mcs.a006096. doi:10.1101/mcs.a006096. PMC 8958913. PMID 34535505.
- ^ a b Cuccurullo C, Cerulli Irelli E, Ugga L, Riva A, D'Amico A, Cabet S, et al. (July 2024). "Clinical features and genotype-phenotype correlations in epilepsy patients with de novo DYNC1H1 variants". Epilepsia. doi:10.1111/epi.18054. PMID 38953796.
- ^ Liu W, Cheng M, Zhu Y, Chen Y, Yang Y, Chen H, et al. (April 2023). "DYNC1H1-related epilepsy: Genotype-phenotype correlation". Developmental Medicine and Child Neurology. 65 (4): 534–543. doi:10.1111/dmcn.15414. PMID 36175372.
Further reading
edit- Narayan D, Desai T, Banks A, Patanjali SR, Ravikumar TS, Ward DC (August 1994). "Localization of the human cytoplasmic dynein heavy chain (DNECL) to 14qter by fluorescence in situ hybridization". Genomics. 22 (3): 660–661. doi:10.1006/geno.1994.1447. PMID 8001984.
- Vaisberg EA, Koonce MP, McIntosh JR (November 1993). "Cytoplasmic dynein plays a role in mammalian mitotic spindle formation". The Journal of Cell Biology. 123 (4): 849–858. doi:10.1083/jcb.123.4.849. PMC 2200153. PMID 8227145.
- Vaughan KT, Mikami A, Paschal BM, Holzbaur EL, Hughes SM, Echeverri CJ, et al. (August 1996). "Multiple mouse chromosomal loci for dynein-based motility". Genomics. 36 (1): 29–38. doi:10.1006/geno.1996.0422. PMID 8812413.
- Bonaldo MF, Lennon G, Soares MB (September 1996). "Normalization and subtraction: two approaches to facilitate gene discovery". Genome Research. 6 (9): 791–806. doi:10.1101/gr.6.9.791. PMID 8889548.
- Nagase T, Ishikawa K, Nakajima D, Ohira M, Seki N, Miyajima N, et al. (April 1997). "Prediction of the coding sequences of unidentified human genes. VII. The complete sequences of 100 new cDNA clones from brain which can code for large proteins in vitro". DNA Research. 4 (2): 141–150. doi:10.1093/dnares/4.2.141. PMID 9205841.
- Neesen J, Koehler MR, Kirschner R, Steinlein C, Kreutzberger J, Engel W, et al. (October 1997). "Identification of dynein heavy chain genes expressed in human and mouse testis: chromosomal localization of an axonemal dynein gene". Gene. 200 (1–2): 193–202. doi:10.1016/S0378-1119(97)00417-4. PMID 9373155.
- Byers HR, Yaar M, Eller MS, Jalbert NL, Gilchrest BA (May 2000). "Role of cytoplasmic dynein in melanosome transport in human melanocytes". The Journal of Investigative Dermatology. 114 (5): 990–997. doi:10.1046/j.1523-1747.2000.00957.x. PMID 10771482.
- Habermann A, Schroer TA, Griffiths G, Burkhardt JK (January 2001). "Immunolocalization of cytoplasmic dynein and dynactin subunits in cultured macrophages: enrichment on early endocytic organelles". Journal of Cell Science. 114 (Pt 1): 229–240. doi:10.1242/jcs.114.1.229. PMID 11112706.
- Sasaki S, Shionoya A, Ishida M, Gambello MJ, Yingling J, Wynshaw-Boris A, et al. (December 2000). "A LIS1/NUDEL/cytoplasmic dynein heavy chain complex in the developing and adult nervous system". Neuron. 28 (3): 681–696. doi:10.1016/S0896-6273(00)00146-X. PMID 11163259.
- Payne C, Rawe V, Ramalho-Santos J, Simerly C, Schatten G (December 2003). "Preferentially localized dynein and perinuclear dynactin associate with nuclear pore complex proteins to mediate genomic union during mammalian fertilization". Journal of Cell Science. 116 (Pt 23): 4727–4738. doi:10.1242/jcs.00784. PMID 14600259. S2CID 20578326.
- Byers HR, Maheshwary S, Amodeo DM, Dykstra SG (October 2003). "Role of cytoplasmic dynein in perinuclear aggregation of phagocytosed melanosomes and supranuclear melanin cap formation in human keratinocytes". The Journal of Investigative Dermatology. 121 (4): 813–820. doi:10.1046/j.1523-1747.2003.12481.x. PMID 14632200.
- Navarro-Lérida I, Martínez Moreno M, Roncal F, Gavilanes F, Albar JP, Rodríguez-Crespo I (February 2004). "Proteomic identification of brain proteins that interact with dynein light chain LC8". Proteomics. 4 (2): 339–346. doi:10.1002/pmic.200300528. PMID 14760703. S2CID 8868600.
- Colland F, Jacq X, Trouplin V, Mougin C, Groizeleau C, Hamburger A, et al. (July 2004). "Functional proteomics mapping of a human signaling pathway". Genome Research. 14 (7): 1324–1332. doi:10.1101/gr.2334104. PMC 442148. PMID 15231748.
- Jin J, Smith FD, Stark C, Wells CD, Fawcett JP, Kulkarni S, et al. (August 2004). "Proteomic, functional, and domain-based analysis of in vivo 14-3-3 binding proteins involved in cytoskeletal regulation and cellular organization". Current Biology. 14 (16): 1436–1450. Bibcode:2004CBio...14.1436J. doi:10.1016/j.cub.2004.07.051. PMID 15324660. S2CID 2371325.
- Andersen JS, Lam YW, Leung AK, Ong SE, Lyon CE, Lamond AI, et al. (January 2005). "Nucleolar proteome dynamics". Nature. 433 (7021): 77–83. Bibcode:2005Natur.433...77A. doi:10.1038/nature03207. PMID 15635413. S2CID 4344740.