The enteric nervous system (ENS) or intrinsic nervous system is one of the three main divisions of the autonomic nervous system (ANS), the others being the sympathetic (SNS) and parasympathetic nervous system (PSNS). It consists of a mesh-like system of neurons that governs the function of the gastrointestinal tract.[1] It is capable of acting independently of the SNS and PSNS, although it may be influenced by them. The ENS is nicknamed the "second brain".[2][3] It is derived from neural crest cells.[4][5]
| Enteric nervous system | |
|---|---|
 The enteric nervous system is embedded in the lining of the gastrointestinal system. | |
| Identifiers | |
| Acronym(s) | ENS |
| MeSH | D017615 |
| FMA | 66070 |
| Anatomical terminology | |
The enteric nervous system is capable of operating independently of the brain and spinal cord,[6] but is thought to rely on innervation from the vagus nerve and prevertebral ganglia in healthy subjects. However, studies have shown that the system is operable with a severed vagus nerve.[7] The neurons of the enteric nervous system control the motor functions of the system, in addition to the secretion of gastrointestinal enzymes. These neurons communicate through many neurotransmitters similar to the CNS, including acetylcholine, dopamine, and serotonin. The large presence of serotonin and dopamine in the intestines are key areas of research for neurogastroenterology.[8][9][10]
Structure
editThe enteric nervous system in humans consists of some 500 million neurons[11] (including the various types of Dogiel cells),[1][12] 0.5% of the number of neurons in the brain, five times as many as the one hundred million neurons in the human spinal cord,[13] and about 2⁄3 as many as in the whole nervous system of a cat. The enteric nervous system is embedded in the lining of the gastrointestinal system, beginning in the esophagus and extending down to the anus.[13]
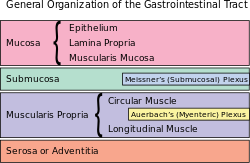
The neurons of the ENS are collected into two types of ganglia: myenteric (Auerbach's) and submucosal (Meissner's) plexuses.[14] Myenteric plexuses are located between the inner and outer layers of the muscularis externa, while submucosal plexuses are located in the submucosa.
Auerbach's plexus
editAuerbach's plexus, also known as the myenteric plexus, is a collection of fibers and postganglionic autonomic cell bodies that lie between the circular and longitudinal layers of the muscularis externa in the gastrointestinal tract.[citation needed] It was discovered and named by German neuropathologist Leopold Auerbach. These neurons provide motor inputs to both layers of the muscularis externa and provide both parasympathetic and sympathetic input. The anatomy of the plexus is similar to the anatomy of the central nervous system. The plexus includes sensory receptors, such as chemoreceptors and mechanoreceptors, that are used to provide sensory input to the interneurons in the enteric nervous system. The plexus is the parasympathetic nucleus of origin for the vagus nerve and communicates with the medulla oblongata through both the anterior and posterior vagal nerves.
Submucosal plexus
editThe submucosal plexus (also known as Meissner's plexus) is found in the submucosal layer of the gastrointestinal tract.[15] It was discovered and named by German physiologist Georg Meissner. It functions as a pathway for the innervation in the mucosa layer of the gastrointestinal wall.
Function
editThe ENS is capable of autonomous functions[16] like the coordination of reflexes; although it receives considerable innervation from the autonomic nervous system, it can and does operate independently of the brain and the spinal cord.[17] Its study is the focus of neurogastroenterology.
Complexity
editThe enteric nervous system has been described as a "second brain" for several reasons. The enteric nervous system can operate autonomously. It normally communicates with the central nervous system (CNS) through the parasympathetic (e.g., via the vagus nerve) and sympathetic (e.g., via the prevertebral ganglia) nervous systems. However, vertebrate studies show that when the vagus nerve is severed, the enteric nervous system continues to function.[7]
In vertebrates, the enteric nervous system includes efferent neurons, afferent neurons, and interneurons, all of which make the enteric nervous system capable of carrying reflexes and acting as an integrating center in the absence of CNS input. The sensory neurons report on mechanical and chemical conditions. Through intestinal muscles, the motor neurons control peristalsis and churning of intestinal contents. Other neurons control the secretion of enzymes. The enteric nervous system also makes use of more than 30 neurotransmitters, most of which are identical to the ones found in CNS, such as acetylcholine, dopamine, and serotonin. More than 90% of the body's serotonin lies in the gut, as well as about 50% of the body's dopamine, which is currently being studied to further our understanding of its utility in the brain.[18][19][20]
The enteric nervous system has the capacity to alter its response depending on such factors as bulk and nutrient composition.[21] In addition, the ENS contains support cells which are similar to astroglia of the brain and a diffusion barrier around the capillaries surrounding ganglia which is similar to the blood–brain barrier of cerebral blood vessels.[22]
Peristalsis
editPeristalsis is a series of radially symmetrical contractions and relaxations of muscles which propagate down a muscular tube. In humans and other mammals, peristalsis is found in the smooth muscles of the digestive tract to propel contents through the digestive system. The word is derived from New Latin and comes from the Greek peristallein, "to wrap around," from peri-, "around" + stallein, "to place". Peristalsis was discovered in 1899 by the work of physiologists William Bayliss and Ernest Starling. Working on the small intestines of dogs, they found that the response of increasing the pressure in the intestine caused the contraction of the muscle wall above the point of stimulation and the relaxation of the muscle wall below the point of stimulation.[23][6]
Segmentation
editSegmentation contractions are the contractions in intestines carried out by the smooth muscle walls. Unlike peristalsis, which involves the contraction and relaxation of muscles in one direction, segmentation occurs simultaneously in both directions as the circular muscles alternatively contract. This allows for thorough mixing of intestinal contents, known as chyme, to allow greater absorption.
Secretion
editThe secretion of gastrointestinal hormones, such as gastrin and secretin, is regulated through cholinergic neurons residing in the walls of the digestive tract. Hormone secretion is controlled by the vagovagal reflex, where the neurons in the digestive tract communicate through both afferent and efferent pathways with the vagus nerve.[24]
Clinical significance
editNeurogastroenterology encompasses the study of the brain, the gut, and their interactions with relevance to the understanding and management of gastrointestinal motility and functional gastrointestinal disorders. Specifically, neurogastroenterology focuses on the functions, malfunctions, and the malformations of the sympathetic, parasympathetic, and enteric divisions of the digestive tract.[25] The term also describes a medical sub-specialism of gastroenterology dedicated to the treatment of motility and functional gastrointestinal disorders.
Functional gastrointestinal disorders
editFunctional gastrointestinal (GI) disorders are a class of gastrointestinal disorders where there is a malfunction in the normal activities of the gastrointestinal tract, but there are no structural abnormalities that can explain the cause. There are rarely any tests that can detect the presence of these disorders. Clinical research in neurogastroenterology focuses mainly on the study of common functional gastrointestinal disorders such as irritable bowel syndrome, the most common functional GI disorder.[26]
Motility disorders
editMotility disorders are the second classification of gastrointestinal disorder studied by neurogastroenterologists. Motility disorders are divided by what they affect, with four regions: The esophagus, the stomach, the small intestines, and the large intestines. Clinical research in neurogastroenterology focuses mainly on the study of common motility disorders such as gastroesophageal reflux disease, the damage of the mucosa of the esophagus caused by rising stomach acid through the lower esophageal sphincter.[27]
Gut ischemia
editENS function can be damaged by ischemia.[28] Transplantation, previously described as a theoretical possibility,[29] has been a clinical reality in the United States since 2011 and is regularly performed at some hospitals.[citation needed]
Additional images
edit-
The myenteric plexus of a rabbit. X 50.
-
The submucosal plexus of a rabbit. X 50.
Neurogastroenterology societies
edit- American Neurogastroenterology and Motility Society[30]
- European Society of Neurogastroenterology and Motility[31]
See also
editReferences
edit- ^ a b Furness JB (15 April 2008). The Enteric Nervous System. John Wiley & Sons. pp. 35–38. ISBN 978-1-4051-7344-5.
- ^ Dorland's (2012). Dorland's Illustrated Medical Dictionary (32nd ed.). Elsevier Saunders. p. 1862. ISBN 978-1-4160-6257-8.
- ^ Pocock G, Richards C (2006). Human Physiology The Basis of Medicine (Third ed.). Oxford University Press. p. 63. ISBN 978-0-19-856878-0.
- ^ Barlow AJ, Wallace AS, Thapar N, Burns AJ (May 2008). "Critical numbers of neural crest cells are required in the pathways from the neural tube to the foregut to ensure complete enteric nervous system formation". Development. 135 (9): 1681–1691. doi:10.1242/dev.017418. PMID 18385256. S2CID 7401456.
- ^ Burns AJ, Thapar N (October 2006). "Advances in ontogeny of the enteric nervous system". Neurogastroenterology and Motility. 18 (10): 876–887. doi:10.1111/j.1365-2982.2006.00806.x. PMID 16961690. S2CID 34066966.
- ^ a b Gershon M (1998). The Second Brain. New York: HarperCollins. pp. 2–7. ISBN 0-06-018252-0.
- ^ a b Li Y, Owyang C (September 2003). "Musings on the wanderer: what's new in our understanding of vago-vagal reflexes? V. Remodeling of vagus and enteric neural circuitry after vagal injury". American Journal of Physiology. Gastrointestinal and Liver Physiology. 285 (3): G461–G469. doi:10.1152/ajpgi.00119.2003. PMID 12909562.
- ^ Pasricha PJ. "Stanford Hospital: Brain in the Gut - Your Health". YouTube.
- ^ Martinucci I, Blandizzi C, de Bortoli N, Bellini M, Antonioli L, Tuccori M, et al. (2015). "Genetics and pharmacogenetics of aminergic transmitter pathways in functional gastrointestinal disorders". Pharmacogenomics. 16 (5): 523–539. doi:10.2217/pgs.15.12. hdl:11577/3166305. PMID 25916523.
- ^ Smitka K, Papezova H, Vondra K, Hill M, Hainer V, Nedvidkova J (2013). "The role of "mixed" orexigenic and anorexigenic signals and autoantibodies reacting with appetite-regulating neuropeptides and peptides of the adipose tissue-gut-brain axis: relevance to food intake and nutritional status in patients with anorexia nervosa and bulimia nervosa". International Journal of Endocrinology. 2013: 483145. doi:10.1155/2013/483145. PMC 3782835. PMID 24106499.
- ^ Young E. "Gut Instincts: The secrets of your second brain". New Scientist. Retrieved 8 April 2015.; alternate source at website: "NeuroScienceStuff". Archived from the original on 4 May 2013.
- ^ p. 921
- ^ a b Hall JE (2011). "General Principles of Gastrointestinal Function". Guyton and Hal Textbook of Medical Physiology (12th ed.). Saunders Elsevier. p. 755. ISBN 978-1416045748.
- ^ "The Enteric Nervous System". Retrieved 29 November 2008.
- ^ Ross, Michael H, and Wojciech Pawlina. Histology: A Text and Atlas with Correlated Cell and Molecular Biology. Baltimore, MD: Lippincott Williams & Wilkins, 2006
- ^ "enteric nervous system" at Dorland's Medical Dictionary
- ^ Gershon, 1998 & 17.
- ^ Pasricha PJ. Brain in the Gut (video). Your Health. Stanford Hospital.
- ^ Martinucci I, Blandizzi C, de Bortoli N, Bellini M, Antonioli L, Tuccori M, et al. (2015). "Genetics and pharmacogenetics of aminergic transmitter pathways in functional gastrointestinal disorders". Pharmacogenomics. 16 (5): 523–539. doi:10.2217/pgs.15.12. hdl:11577/3166305. PMID 25916523.
- ^ Smitka K, Papezova H, Vondra K, Hill M, Hainer V, Nedvidkova J (2013). "The role of "mixed" orexigenic and anorexigenic signals and autoantibodies reacting with appetite-regulating neuropeptides and peptides of the adipose tissue-gut-brain axis: relevance to food intake and nutritional status in patients with anorexia nervosa and bulimia nervosa". International Journal of Endocrinology. 2013: 483145. doi:10.1155/2013/483145. PMC 3782835. PMID 24106499.
- ^ Neunlist M, Schemann M (July 2014). "Nutrient-induced changes in the phenotype and function of the enteric nervous system". The Journal of Physiology. 592 (14). Wiley: 2959–2965. doi:10.1113/jphysiol.2014.272948. PMC 4214652. PMID 24907307. S2CID 37969390.
- ^ Silverthorn DU (2007). Human Physiology. San Francisco, CA: Pearson Education, Inc.
- ^ Keet AS. "The Pyloric Sphincteric Cylinder in health and disease". Retrieved 18 November 2013.
- ^ Herman MA, Cruz MT, Sahibzada N, Verbalis J, Gillis RA (January 2009). "GABA signaling in the nucleus tractus solitarius sets the level of activity in dorsal motor nucleus of the vagus cholinergic neurons in the vagovagal circuit". American Journal of Physiology. Gastrointestinal and Liver Physiology. 296 (1): G101–G111. doi:10.1152/ajpgi.90504.2008. PMC 2636929. PMID 19008339.
- ^ Wood JD, Alpers DH, Andrews PL (September 1999). "Fundamentals of neurogastroenterology". Gut. 45 (Suppl 2): II6–II16. doi:10.1136/gut.45.2008.ii6. PMC 1766686. PMID 10457039.
- ^ Kumar A, Rinwa P, Sharma N (2012). "Irritable Bowel Syndrome: A Review". J Phys Pharm Adv. 2 (2): 97–108.
- ^ DeVault KR, Castell DO (June 1999). "Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. The Practice Parameters Committee of the American College of Gastroenterology". The American Journal of Gastroenterology. 94 (6): 1434–1442. doi:10.1111/j.1572-0241.1999.1123_a.x. PMID 10364004. S2CID 32509777.
- ^ Linhares GK, Martins JL, Fontanezzi F, Patrício F, Montero EF (2007). "Do lesions of the enteric nervous system occur following intestinal ischemia/reperfusion?". Acta Cirurgica Brasileira. 22 (2): 120–124. doi:10.1590/S0102-86502007000200008. PMID 17375218.
- ^ Gershon MD (April 2007). "Transplanting the enteric nervous system: a step closer to treatment for aganglionosis". Gut. 56 (4): 459–461. doi:10.1136/gut.2006.107748. PMC 1856867. PMID 17369379.
- ^ ANMS - American Neurogastroenterology and Motility Society
- ^ ESNM - European Society for Neurogastroenterology & Motility
Further references
edit- Grosell M, Farrell AP, Brauner CJ, eds. (2010). Fish Physiology: The Multifunctional Gut of Fish. Academic Press. ISBN 978-0-08-096136-1.
- Gershon MD (1999). The Second Brain: A Groundbreaking New Understanding of Nervous Disorders of the Stomach and Intestine. Harper Perennial. ISBN 978-0-06-093072-1.
- Nosek TM. "Section 6/6ch2/s6ch2_29". Essentials of Human Physiology. Archived from the original on 2016-03-24.