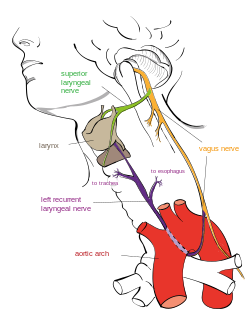
The recurrent laryngeal nerve (RLN) is a branch of the vagus nerve (cranial nerve X) that supplies all the intrinsic muscles of the larynx, with the exception of the cricothyroid muscles. There are two recurrent laryngeal nerves, right and left. The right and left nerves are not symmetrical, with the left nerve looping under the aortic arch, and the right nerve looping under the right subclavian artery, then traveling upwards. They both travel alongside the trachea. Additionally, the nerves are among the few nerves that follow a recurrent course, moving in the opposite direction to the nerve they branch from, a fact from which they gain their name.
| Recurrent laryngeal nerve | |
|---|---|
 Course of the left recurrent laryngeal nerve | |
 | |
| Details | |
| From | Vagus nerve |
| Innervates | Larynx posterior cricoarytenoid lateral cricoarytenoid arytenoid thyroarytenoid aryepiglottis esophagus heart trachea inferior pharyngeal constrictor muscle |
| Identifiers | |
| Latin | nervus laryngeus recurrens |
| MeSH | D012009 |
| TA98 | A14.2.01.166 |
| TA2 | 6344 |
| FMA | 6246 |
| Anatomical terms of neuroanatomy | |
The recurrent laryngeal nerves supply sensation to the larynx below the vocal cords, give cardiac branches to the deep cardiac plexus, and branch to the trachea, esophagus and the inferior constrictor muscles. The posterior cricoarytenoid muscles, the only muscles that can open the vocal folds, are innervated by this nerve.
The recurrent laryngeal nerves are the nerves of the sixth pharyngeal arch. The existence of the recurrent laryngeal nerve was first documented by the physician Galen.
Structure
editThe recurrent laryngeal nerves branch from the vagus nerve, relative to which they get their names; the term "recurrent" from Latin: re- (back) and currere (to run),[1] indicates they run in the opposite direction to the vagus nerves from which they branch.[2] The vagus nerves run down into the thorax, and the recurrent laryngeal nerves run up to the larynx.[3]: 930–931
The vagus nerves, from which the recurrent laryngeal nerves branch, exit the skull at the jugular foramen and travel within the carotid sheath alongside the carotid arteries through the neck. The recurrent laryngeal nerves branch off the vagus, the left at the aortic arch, and the right at the right subclavian artery. The left RLN passes in front of the arch, and then wraps underneath and behind it. After branching, the nerves typically ascend in a groove at the junction of the trachea and esophagus.[4]: 1346–1347 They then pass behind the posterior, middle part of the outer lobes of the thyroid gland and enter the larynx underneath the inferior constrictor muscle,[3]: 918 passing into the larynx just posterior to the cricothyroid joint.[5] The terminal branch is called the inferior laryngeal nerve.[6]: 19
Unlike the other nerves supplying the larynx, the right and left RLNs lack bilateral symmetry.[7] The left RLN is longer than the right, because it crosses under the arch of the aorta at the ligamentum arteriosum.[4]: 1346–1347
Nucleus
editThe somatic motor fibers that innervate the laryngeal muscles, and pharyngeal muscles are located in the nucleus ambiguus and emerge from the medulla in the cranial root of the accessory nerve. Fibers cross over to and join the vagus nerve in the jugular foramen.[8]: 86–88 Sensory cell bodies are located in the inferior jugular ganglion,[9] and the fibers terminate in the solitary nucleus.[8]: 86–88 Parasympathetic fibers to segments of the trachea and esophagus in the neck originate in the dorsal nucleus of the vagus nerve.[9]
Development
editDuring human and all vertebrate development, a series of pharyngeal arch pairs form in the developing embryo. These project forward from the back of the embryo towards the front of the face and neck. Each arch develops its own artery, nerve that controls a distinct muscle group, and skeletal tissue. The arches are numbered from 1 to 6, with 1 being the arch closest to the head of the embryo, and the fifth arch only existing transiently.[10]: 318–323
Arches 4 and 6 produce the laryngeal cartilages. The nerve of the sixth arch becomes the recurrent laryngeal nerve. The nerve of the fourth arch gives rise to the superior laryngeal nerve. The arteries of the fourth arch, which project between the nerves of the fourth and sixth arches, become the left-sided arch of the aorta and the right subclavian artery. The arteries of the sixth arch persist as the ductus arteriosus on the left, and are obliterated on the right.[10]: 318–323
After birth, the ductus arteriosus regresses to form the ligamentum arteriosum. During growth, these arteries descend into their ultimate positions in the chest, creating the elongated recurrent paths.[10]: 318–323
Variation
editIn roughly 1 out of every 100–200 people, the right inferior laryngeal nerve is nonrecurrent, branching off the vagus nerve around the level of the cricoid cartilage. Typically, such a configuration is accompanied by variation in the arrangement of the major arteries in the chest; most commonly, the right subclavian artery arises from the left side of the aorta and crosses behind the esophagus. A left nonrecurrent inferior laryngeal nerve is even more uncommon, requiring the aortic arch be on the right side, accompanied by an arterial variant which prevents the nerve from being drawn into the chest by the left subclavian.[11]: 10, 48
In about four people out of five, there is a connecting branch between the inferior laryngeal nerve, a branch of the RLN, and the internal laryngeal nerve, a branch of the superior laryngeal nerve. This is commonly called the anastomosis of Galen (Latin: ansa galeni), even though anastomosis usually refers to a blood vessel,[12][13]: 35 and is one of several documented anastomoses between the two nerves.[14]
As the recurrent nerve hooks around the subclavian artery or aorta, it gives off several branches. There is suspected variability in the configuration of these branches to the cardiac plexus, trachea, esophagus and inferior pharyngeal constrictor muscle.[15]
Function
editThe recurrent laryngeal nerves control all intrinsic muscles of the larynx except for the cricothyroid muscle.[15][a] These muscles act to open, close, and adjust the tension of the vocal cords, and include the posterior cricoarytenoid muscles, the only muscle to open the vocal cords.[16]: 10–11 The nerves supply muscles on the same side of the body, with the exception of the interarytenoid muscle, which is innervated from both sides.[15]
The nerves also carry sensory information from the mucous membranes of the larynx below the lower surface of the vocal fold,[17]: 847–9 as well as sensory, secretory and motor fibres to the cervical segments of the esophagus and the trachea.[8]: 142–144
Clinical significance
editInjury
editThe recurrent laryngeal nerves may be injured as a result of trauma, during surgery, as a result of tumour spread, or due to other means.[16]: 12 Injury to the recurrent laryngeal nerves can result in a weakened voice (hoarseness) or loss of voice (aphonia) and cause problems in the respiratory tract.[18][16]: 11–12 Injury to the nerve may paralyze the posterior cricoarytenoid muscle on the same side. This is the sole muscle responsible for opening the vocal cords, and paralysis may cause difficulty breathing (dyspnea) during physical activity.[19] Injury to both the right and left nerve may result in more serious damage, such as the inability to speak. Additional problems may emerge during healing, as nerve fibres that re-anastamose may result in vocal cord motion impairment, uncoordinated movements of the vocal cord.[16]: 12–13
Surgery
editThe nerve receives close attention from surgeons because the nerve is at risk for injury during neck surgery, especially thyroid and parathyroid surgery; as well as esophagectomy.[20][4] Nerve damage can be assessed by laryngoscopy, during which a stroboscopic light confirms the absence of movement in the affected side of the vocal cords. The right recurrent laryngeal nerve is more susceptible to damage during thyroid surgery because it is close to the bifurcation of the right inferior thyroid artery, variably passing in front of, behind, or between the branches.[17]: 820–1 Similarly, thermal injury can occur with the use of radio frequency ablation to remove thyroid nodules.[21][22][23] The nerve is permanently damaged in 0.3–3% of thyroid surgeries, and transient paralysis occurs in 3–8% of surgeries; accordingly, recurrent laryngeal nerve damage is one of the leading causes of medicolegal issues for surgeons.[24] A 2019 systematic review concluded that the available evidence shows no difference between visually identifying the nerve or utilizing intraoperative neuroimaging during surgery, when trying to prevent injury to recurrent laryngeal nerve during surgery.[25]
Tumors
editThe RLN may be compressed by tumors. Studies have shown that 2–18% of lung cancer patients develop hoarseness because of recurrent laryngeal nerve compression, usually left-sided.[26] This is associated with worse outcomes, and when found as a presenting symptom, often indicates inoperable tumors. The nerve may be severed intentionally during lung cancer surgery in order to fully remove a tumor.[27]: 330 The RLN may also be damaged by tumors in the neck, especially with malignant lymph nodes with extra-capsular extension of tumor beyond the capsule of the nodes, which may invade the area that carries the ascending nerve on the right or left.
Other disease
editIn Ortner's syndrome or cardiovocal syndrome, a rare cause of left recurrent laryngeal nerve palsy, expansion of structures within the heart or major blood vessels impinges upon the nerve, causing symptoms of unilateral nerve injury.[28]
Other animals
editHorses are subject to equine recurrent laryngeal neuropathy, a disease of the axons of the recurrent laryngeal nerves. The cause is not known, although a genetic predisposition is suspected. The length of the nerve is a factor since it is more common in larger horses, and the left side is affected almost exclusively. As the nerve cells die, there is a progressive paralysis of the larynx, causing the airway to collapse. The common presentation is a sound, ranging from a musical whistle to a harsh roar or heaving gasping noise (stertorous), accompanied by worsening performance. The condition is incurable, but surgery can keep the airway open. Experiments with nerve grafts have been tried.[29]: 421–426
Although uncommon in dogs, bilateral recurrent laryngeal nerve disease may be the cause of wheezing (stridor) when middle-aged dogs inhale.[30]: 771
In sauropod dinosaurs, the vertebrates with the longest necks, the total length of the vagus nerve and recurrent laryngeal nerve would have been up to 28 metres (92 ft) long in Supersaurus, but these would not be the longest neurons that ever existed: the neurons reaching the tip of the tail would have exceeded 30 metres (98 ft).[31]
Evidence of evolution
editThe extreme detour of the recurrent laryngeal nerves, about 4.6 metres (15 ft) in the case of giraffes,[32]: 74–75 is cited as evidence of evolution, as opposed to intelligent design. The nerve's route would have been direct in the fish-like ancestors of modern tetrapods, traveling from the brain, past the heart, to the gills (as it does in modern fish). Over the course of evolution, as the neck extended and the heart became lower in the body, the laryngeal nerve remained in its original course.
History
editAncient Greek physician Galen demonstrated the nerve course and the clinical syndrome of recurrent laryngeal nerve paralysis, noting that pigs with the nerve severed were unable to squeal. Galen named the nerve the recurrent nerve, and described the same effect in two human infants who had undergone surgery for goiter.[16]: 7–8 [33] In 1838, five years before he would introduce the concept of homology to biology, anatomist Richard Owen reported upon the dissection of three giraffes, including a description of the full course of the left recurrent laryngeal nerve.[34][35] Anatomists Andreas Vesalius and Thomas Willis described the nerve in what is now regarded as an anatomically standard description, and doctor Frank Lahey documented a way for its interoperative identification during thyroid operations.[36]
Notes
editReferences
edit- ^ "Recur". Free Dictionary. Merriam-Webster. Retrieved March 1, 2013.
- ^ "Recurrent". Medical definition and more. Merriam-Webster. Retrieved March 1, 2013.
- ^ a b Drake RL, Vogl W, Mitchell AW (2005). Gray's Anatomy for Students. Philadelphia: Elsevier/Churchill Livingstone. ISBN 978-0-8089-2306-0.
- ^ a b c Brunicardi FC, Brunicardi F, Andersen D, Raphael EP, Billiar T, Dunn D, et al. (September 11, 2009). Schwartz's Principles of Surgery (9th ed.). McGraw Hill Professional. ISBN 978-0-07-154769-7.
- ^ Agur, A. M. R.; Dalley, Arthur F. (2009). Grant's Atlas of Anatomy. Lippincott Williams & Wilkins. p. 770. ISBN 978-0-7817-7055-2.
- ^ Ross, Lawrence M.; Lamperti, Edward D. (2006). Thieme Atlas of Anatomy: Neck and Internal Organs. Thieme. ISBN 978-1-58890-443-0.
- ^ Aronson, Arnold Elvin (2009). Clinical Voice Disorders. Thieme. p. 74. ISBN 978-1-58890-662-5.
- ^ a b c Schulte E, Schumacher U, Rude J (2007). Thieme Atlas of Anatomy: Head and Neuroanatomy. Thieme. ISBN 978-1-58890-441-6.
- ^ a b Alberstone, Cary D. (2009). Anatomic Basis of Neurologic Diagnosis. Thieme. pp. 260–261. ISBN 978-0-86577-976-1.
- ^ a b c Larsen, William J. (1993). Human embryology. Churchill Livingstone. ISBN 0-443-08724-5. Retrieved February 26, 2013.
- ^ Duh QY, Clark OH, Kebebew E (October 14, 2009). Atlas of Endocrine Surgical Techniques. Elsevier Health Sciences. ISBN 978-1-4160-4844-2. Retrieved March 6, 2013.
- ^ Naidu L, Ramsaroop L, Partab P, Satyapal KS (September 2012). "Galen's "anastomosis" revisited". Clinical Anatomy. 25 (6): 722–728. doi:10.1002/ca.22011. PMID 22162120. S2CID 23512491.
- ^ Langmore SE (January 2001). Endoscopic Evaluation and Treatment of Swallowing Disorders. Thieme. ISBN 978-0-86577-838-2.
- ^ Sañudo JR, Maranillo E, León X, Mirapeix RM, Orús C, Quer M (June 1999). "An anatomical study of anastomoses between the laryngeal nerves". The Laryngoscope. 109 (6): 983–987. doi:10.1097/00005537-199906000-00026. PMID 10369294. S2CID 26161510.
- ^ a b c "Laryngeal Nerve Anatomy: Introduction, Vagus Nerve (Cranial Nerve X), Superior Laryngeal Nerve". 28 November 2023. Retrieved 3 August 2024.
- ^ a b c d e Hydman J (2008). Recurrent laryngeal nerve injury. Stockholm. ISBN 978-91-7409-123-6.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ a b Moore KL (1992). Clinically Oriented Anatomy (3rd ed.). Williams & Wilkins. ISBN 0-683-06133-X.
- ^ Aljammal J, Hussain I, Ahmad S (2022-03-01). "Management of Recurrent Laryngeal Nerve Injury During Radiofrequency Ablation of Thyroid Nodules". AACE Clinical Case Reports. 8 (2): 102. doi:10.1016/j.aace.2022.02.004. PMC 8984510. PMID 35415225.
- ^ Hartl DM, Travagli JP, Leboulleux S, Baudin E, Brasnu DF, Schlumberger M (May 2005). "Clinical review: Current concepts in the management of unilateral recurrent laryngeal nerve paralysis after thyroid surgery". The Journal of Clinical Endocrinology and Metabolism. 90 (5): 3084–3088. doi:10.1210/jc.2004-2533. PMID 15728196.
- ^ Yamamoto, Natsuhiro, Yamaguchi, Yoshikazu, Nomura, Takeshi, et al. Successful Assessment of Vocal Cord Palsy Before Tracheal Extubation by Laryngeal Ultrasonography in a Patient After Esophageal Surgery: A Case Report. A&A Case Reports. 2017;9(11):308-310. doi:10.1213/XAA.0000000000000601.
- ^ Hussain I, Zulfiqar F, Li X, Ahmad S, Aljammal J (August 2021). "Safety and Efficacy of Radiofrequency Ablation of Thyroid Nodules-Expanding Treatment Options in the United States". Journal of the Endocrine Society. 5 (8): bvab110. doi:10.1210/jendso/bvab110. PMC 8271212. PMID 34258495.
- ^ Muhammad H, Santhanam P, Russell JO (June 2021). "Radiofrequency ablation and thyroid nodules: updated systematic review". Endocrine. 72 (3): 619–632. doi:10.1007/s12020-020-02598-6. PMID 33449296. S2CID 231611505.
- ^ Allen E, Minutello K, Murcek BW (2022). "Anatomy, Head and Neck, Larynx Recurrent Laryngeal Nerve". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 29261997. Retrieved 2022-05-24.
- ^ Hayward NJ, Grodski S, Yeung M, Johnson WR, Serpell J (January 2013). "Recurrent laryngeal nerve injury in thyroid surgery: a review". ANZ Journal of Surgery. 83 (1–2): 15–21. doi:10.1111/j.1445-2197.2012.06247.x. PMID 22989215. S2CID 8581189.
- ^ Cirocchi R, Arezzo A, D'Andrea V, Abraha I, Popivanov GI, Avenia N, et al. (Cochrane Metabolic and Endocrine Disorders Group) (January 2019). "Intraoperative neuromonitoring versus visual nerve identification for prevention of recurrent laryngeal nerve injury in adults undergoing thyroid surgery". The Cochrane Database of Systematic Reviews. 1 (1): CD012483. doi:10.1002/14651858.CD012483.pub2. PMC 6353246. PMID 30659577.
- ^ Spiro SG, Gould MK, Colice GL (September 2007). "Initial evaluation of the patient with lung cancer: symptoms, signs, laboratory tests, and paraneoplastic syndromes: ACCP evidenced-based clinical practice guidelines (2nd edition)". Chest. 132 (3 Suppl): 149S–160S. doi:10.1378/chest.07-1358. PMID 17873166.
- ^ Carbone DP, Pass HI, Johnson DH, Minna JD (2010). Principles and Practice of Lung Cancer: The Official Reference Text of the IASLC. Lippincott Williams & Wilkins. ISBN 978-0-7817-7365-2. Retrieved August 12, 2013.
- ^ Heikkinen J, Milger K, Alejandre-Lafont E, Woitzik C, Litzlbauer D, Vogt JF, et al. (2012). "Cardiovocal Syndrome (Ortner's Syndrome) Associated with Chronic Thromboembolic Pulmonary Hypertension and Giant Pulmonary Artery Aneurysm: Case Report and Review of the Literature". Case Reports in Medicine. 2012: 230736. doi:10.1155/2012/230736. PMC 3477763. PMID 23424588.
- ^ Munroe G, Weese S (March 15, 2011). Equine Clinical Medicine, Surgery and Reproduction. Manson Publishing. ISBN 978-1-84076-608-0. Retrieved March 2, 2013.
- ^ Slatter DH (2003). Textbook of Small Animal Surgery. Elsevier Health Sciences. ISBN 978-0-7216-8607-3. Retrieved March 2, 2013.
- ^ Wedel MJ (June 2012). "A Monument of Inefficiency: The Presumed Course of the Recurrent Laryngeal Nerve in Sauropod Dinosaurs". Acta Palaeontologica Polonica. 57 (2): 251–256. doi:10.4202/app.2011.0019.
- ^ Mammal Anatomy: An Illustrated Guide. Marshall Cavendish Corporation. 2010. ISBN 978-0-7614-7882-9.
- ^ Gross CG (May 1998). "Galen and the Squealing Pig". Neuroscientist. 4 (3): 216–221. doi:10.1177/107385849800400317. ISSN 1073-8584. S2CID 72125962.
- ^ Owen R (1841). "Notes on the dissection of the Nubian giraffe". Transactions of the Zoological Society of London. Zoological Society of London. pp. 217–248. Retrieved February 27, 2013.
- ^ Berry RJ, Hallam A (1986). The Collins Encyclopedia of Animal Evolution. HarperCollins Publishers Limited. pp. 82–83. ISBN 978-0-00-219818-9. Retrieved February 27, 2013.
- ^ Ardito G, Revelli L, D'Alatri L, Lerro V, Guidi ML, Ardito F (February 2004). "Revisited anatomy of the recurrent laryngeal nerves". American Journal of Surgery. 187 (2): 249–253. doi:10.1016/j.amjsurg.2003.11.001. PMID 14769313.
External links
edit- Anatomy figure: 21:04-01 at Human Anatomy Online, SUNY Downstate Medical Center
- cranialnerves at The Anatomy Lesson by Wesley Norman (Georgetown University) (X)
- Dissection of a giraffe displaying the laryngeal nerve (youTube)