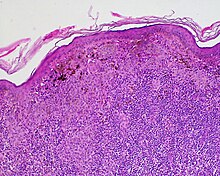
Halo nevus is a mole that is surrounded by a pale ring or 'halo'.[1] It is generally noticed in the summer, when surrounding skin tans, and usually occurs on the chest, but can be anywhere.[1] There may be one or more typically several.[2] Onset is usually in teenagers and young adults.[1][3] It typically follows a pattern of appearing at first as a dark mole surrounded by a halo before the nevus fades and disappears.[1] A single halo nevus like lesion appearing in an older adult may be a melanoma.[1]
| Halo nevus | |
|---|---|
| Other names | Leukoderma acquisitum centrifugum of sutton |
 | |
| Specialty | Dermatology |
It occurs in around 1% of general population, and males and females are affected equally.[1]
Presentation
editHalo nevi are also known as Sutton's nevi, or leukoderma acquisitum centrifugum.[2] Halo nevi are named such because they are a mole (nevus) that is surrounded by an area of depigmentation that resembles a halo.
Halo nevi are associated with vitiligo. Sometimes the pale (hypopigmented) areas will spontaneously regress, and pigment returns.
Causes
editThe formation of a halo surrounding a nevi is believed to occur when certain white blood cells called CD8+ T lymphocytes destroy the pigment-producing cells of the skin (melanocytes).[4] The cause for the attack is unknown.[5]
Diagnosis
editThis section is empty. You can help by adding to it. (February 2018) |
Treatment
editAs halo nevi are only of cosmetic significance, no treatment is required,[6] and patients will be asymptomatic. Although halo nevi are harmless, it is important to monitor the lesion on regular basis.[7] Watch out for any changes in appearance of existing or new halo nevi. If there is any change in appearance or is associated with pain, itch, and infection, a doctor should be consulted immediately to exclude the possibility of melanoma.
Epidemiology
editHalo nevi are estimated to be present in approximately 1% of the general population, and are found to be more prevalent in people with vitiligo, malignant melanoma,[5] or Turner syndrome.[8] All races and sexes are equally susceptible to this disease, although a familial tendency has been reported. The average age of onset is in a person's teenage years.
See also
editReferences
edit- ^ a b c d e f DE, Elder; D, Massi; RA, Scolyer; R, Willemze (2018). "2. Melanocytic tumours: halo naevus". WHO Classification of Skin Tumours. Vol. 11 (4th ed.). Lyon (France): World Health Organization. pp. 91–92. ISBN 978-92-832-2440-2.
- ^ a b James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "30. Melanocytic nevi and neoplasms: halo nevus". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. pp. 690–691. ISBN 978-0-323-54753-6.
- ^ Johnstone, Ronald B. (2017). "32. Lentigines, nevi and melanomas". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. p. 536. ISBN 978-0-7020-6830-0.
- ^ Mundinger, Gerhard S. (January 16, 2014). "Halo Phenomenon". New England Journal of Medicine. 370 (3): 262. doi:10.1056/NEJMicm1306230. PMID 24428471.
- ^ a b "Halo Nevus - skinsite.com". Retrieved August 4, 2008.
- ^ "CareFair.com - Halo Nevis". Retrieved August 4, 2008.
- ^ "DermaTalk - Halo Nevus".
- ^ Halo Nevis at eMedicine
External links
edit