Staphylococcus epidermidis
Staphylococcus epidermidis is a Gram-positive bacterium, and one of over 40 species belonging to the genus Staphylococcus.[1] It is part of the normal human microbiota, typically the skin microbiota, and less commonly the mucosal microbiota and also found in marine sponges.[2][3] It is a facultative anaerobic bacteria. Although S. epidermidis is not usually pathogenic, patients with compromised immune systems are at risk of developing infection. These infections are generally hospital-acquired.[4] S. epidermidis is a particular concern for people with catheters or other surgical implants because it is known to form biofilms that grow on these devices.[5] Being part of the normal skin microbiota, S. epidermidis is a frequent contaminant of specimens sent to the diagnostic laboratory.[6]
| Staphylococcus epidermidis | |
|---|---|
| |
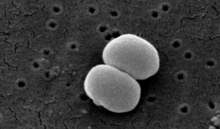
| Scanning electron image of S. epidermidis. | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Bacillota |
| Class: | Bacilli |
| Order: | Caryophanales |
| Family: | Staphylococcaceae |
| Genus: | Staphylococcus |
| Species: | S. epidermidis
|
| Binomial name | |
| Staphylococcus epidermidis (Winslow & Winslow 1908)
Evans 1916 | |
| Synonyms | |
|
Staphylococcus albus Rosenbach 1884 | |
Some strains of S. epidermidis are highly salt tolerant and commonly found in marine environment.[3] S.I. Paul et al. (2021)[3] isolated and identified salt tolerant strains of S. epidermidis (strains ISP111A, ISP111B and ISP111C) from Cliona viridis sponges of the Saint Martin's Island Area of the Bay of Bengal, Bangladesh.
Commensal S. epidermidis is an essential part of a healthy skin microbiota. It contributes through supporting a healthy skin barrier, healing cuts of the skin, protecting the skin microbiota from colonization of skin pathogens, and acting as an immune system modulator.[7]

Etymology
edit'Staphylococcus' - bunch of grape-like berries, 'epidermidis' - of the epidermis.[8]
Discovery
editFriedrich Julius Rosenbach distinguished S. epidermidis from S. aureus in 1884, initially naming S. epidermidis as S. albus.[9] He chose aureus and albus since the bacteria formed yellow and white colonies, respectively.
Microbiology
editStaphylococcus epidermidis is a very hardy microorganism, consisting of nonmotile, Gram-positive cocci, arranged in grape-like clusters. It forms white, raised, cohesive colonies about 1–2 mm in diameter after overnight incubation, and is not hemolytic on blood agar.[5] It is a catalase-positive,[10] coagulase-negative, facultative anaerobe that can grow by aerobic respiration or by fermentation. Some strains may not ferment.[3][11]
Biochemical tests indicate this microorganism also carries out a weakly positive reaction to the nitrate reductase test. It is positive for urease production, is oxidase negative, and can use glucose, sucrose, and lactose to form acid products. In the presence of lactose, it will also produce gas. Nonpathogenic S. epidermidis unlike pathogenic S. aureus does not possess the gelatinase enzyme, so it cannot hydrolyze gelatin.[12][13] It is sensitive to novobiocin, providing an important test to distinguish it from Staphylococcus saprophyticus, which is coagulase-negative, as well, but novobiocin-resistant.[4]
Similar to those of S. aureus, the cell walls of S. epidermidis have a transferrin-binding protein that helps the organism obtain iron from transferrin. The tetramers of a surface exposed protein, glyceraldehyde-3-phosphate dehydrogenase, are believed to bind to transferrin and remove its iron. Subsequent steps include iron being transferred to surface lipoproteins, then to transport proteins which carry the iron into the cell.[5]
Biochemical characteristics
editColony, morphological, physiological, and biochemical characteristics of marine S. epidermidis are shown in the table below.[3]
| Test type | Test | Characteristics |
|---|---|---|
| Colony characters | Size | Pin headed/ Very small |
| Type | Round | |
| Color | Opaque | |
| Shape | Convex | |
| Morphological characters | Shape | Cocci |
| Physiological characters | Motility | – |
| Growth at 6.5% NaCl | + | |
| Biochemical characters | Gram's staining | + |
| Oxidase | – | |
| Catalase | + | |
| Oxidative-Fermentative | Fermentative | |
| Motility | – | |
| Methyl Red | – | |
| Voges-Proskauer | + | |
| Indole | – | |
| H2S Production | + | |
| Urease | + | |
| Nitrate reductase | + | |
| β-Galactosidase | + | |
| Hydrolysis of | Gelatin | – |
| Aesculin | + | |
| Casein | + | |
| Tween 40 | + | |
| Tween 60 | + | |
| Tween 80 | + | |
| Acid production from | Glycerol | – |
| Galactose | W | |
| D-Glucose | + | |
| D-Fructose | + | |
| D-Mannose | + | |
| Mannitol | – | |
| N-Acetylglucosamine | + | |
| Amygdalin | + | |
| Maltose | + | |
| D-Melibiose | + | |
| D-Trehalose | + | |
| Glycogen | + | |
| D-Turanose | + |
Note: + = Positive, – = Negative, W = Weakly Positive
Identification
editThe normal practice of detecting S. epidermidis is by using appearance of colonies on selective media, bacterial morphology by light microscopy, catalase and slide coagulase testing. Zobell agar is useful for the isolation of Staphylococcus epidermidis from marine organisms.[3] On the Baird-Parker agar with egg yolk supplement, colonies appear small and black. Increasingly, techniques such as quantitative PCR are being employed for the rapid detection and identification of Staphylococcus strains.[14][15] Normally, sensitivity to desferrioxamine can also be used to distinguish it from most other staphylococci, except in the case of Staphylococcus hominis, which is also sensitive.[16] In this case, the production of acid from trehalose by S. hominis can be used to tell the two species apart.[citation needed]
Microbial ecology
editRole in foot odor
editA common misconception about foot odor and body odor in general is that sweat itself smells and causes people to smell. However, sweat itself is almost entirely odorless. Rather, microbes present on the skin metabolize certain compounds in sweat as a source of nutrients, producing compounds with an unpleasant smell in the process.[17] S. epidermidis thrives in warm, moist environments and is a common bacteria of the human microbiome;[18] it is thus primarily responsible for foot odor as feet have more sweat glands than any other part of the body and thus are often moist, which creates an ideal environment for S. epidermidis to thrive. The bacteria produces enzymes that degrade the leucine present in sweat, producing unpleasant smelling volatile compounds such as isovaleric acid. Feet with stronger odors have a higher density of microorganisms than those with weaker foot odor.[18]
Role in disease
editVirulence factors
editBiofilm formation
editS. epidermidis causes biofilms to grow on plastic devices placed within the body.[19] This occurs most commonly on intravenous catheters and on medical prostheses.[20] Infection can also occur in dialysis patients or anyone with an implanted plastic device that may have been contaminated. It also causes endocarditis, most often in patients with defective heart valves. In some other cases, sepsis can occur in hospital patients. [citation needed]
The ability to form biofilms on plastic devices is a major virulence factor for S. epidermidis. One probable cause is surface proteins that bind blood and extracellular matrix proteins. It produces an extracellular material known as polysaccharide intercellular adhesin (PIA), which is made up of sulfated polysaccharides. It allows other bacteria to bind to the already existing biofilm, creating a multilayer biofilm. Such biofilms decrease the metabolic activity of bacteria within them. This decreased metabolism, in combination with impaired diffusion of antibiotics, makes it difficult for antibiotics to effectively clear this type of infection.[5]
Antibiotics are largely ineffective in clearing biofilms. The most common treatment for these infections is to remove or replace the infected implant, though in all cases, prevention is ideal. The drug of choice is often vancomycin, to which rifampin or an aminoglycoside can be added.[citation needed] Hand washing has been shown to reduce the spread of infection.
Antibiotic resistance
editS. epidermidis strains are often resistant to antibiotics, including rifamycin, fluoroquinolones, gentamicin, tetracycline, clindamycin, and sulfonamides.[19] Methicillin resistance is particularly widespread, with 75-90% of hospital isolates resistance to methicillin.[19] Resistant organisms are most commonly found in the intestine, but organisms living on the skin can also become resistant due to routine exposure to antibiotics secreted in sweat.[citation needed]
Acne vulgaris
editPreliminary research also indicates S. epidermidis is universally found inside affected acne vulgaris pores, where Cutibacterium acnes is normally the sole resident.[21]
Staphylococcus epidermidis in the normal skin is nonpathogenic. But in abnormal lesions, it becomes pathogenic, likely in acne vulgaris. Staphylococcus epidermidis enters the sebaceous gland (colonized by Propionibacterium acnes, the main bacterium that causes acne vulgaris) and damages the hair follicles by producing lipolytic enzymes that change the sebum from fraction to dense (thick) form leading to inflammatory effect.[22]
Moreover, S. epidermidis biofilm formation by releasing the exopolysaccharide intercellular adhesion (PIA) provides the susceptible anaerobic environment to P. acnes colonisation and protects it from the innate human immunity molecules.[23]
Both P. acnes and S. epidermidis can interact to protect the host skin health from pathogens colonisation. But in the case of competition, they use the same carbon source (i.e. glycerol) to produce short chain fatty acids which act as antibacterial agent against each other. Also, S. epidermidis helps in skin homeostasis and reduces the P. acnes pathogenic inflammation by decreasing the TLR2 protein production that induces the skin inflammation.[24]
Role in skin health
editSkin barrier reinforcement
editCommensal S. epidermidis also has been shown to contribute to skin barrier homeostasis through the generation of protective ceramides, which helps maintain the integrity of the skin barrier. By modulating the moist, inner lining of some organs and body cavities and their specific immune defense mechanisms, skin commensals interact with infectious agents like pathogens. Sphingomyelin phosphodiesterase is the main driver in the S. epidermidis production of ceramides - a lipid that includes sphingosine and sphingosine-1-phosphate. This lipid, both obtains nutrients essential for bacteria and helps the host in the production of ceramides. Ceramides are important components of the epithelial barrier, and they play a key role in preventing skin from losing moisture; this acts as a protectant and averts against both dehydration and aging of the skin.[25]
Metabolic interaction
editS. epidermidis plays a key role in metabolic processes that influence skin conditions. The bacterium can affect biochemical pathways within skin cells, which can impact skin health and disease states. Specifically, this is seen in the modulation of the aryl hydrocarbon receptor.[7]
In non-atopic skin, S. epidermidis will help communicate the activation of the aryl hydrocarbon receptor pathway, which both enhances the skin barrier function and helps reduce inflammation. Atopic skin will usually have the inverse effect by acting as a blocker of this pathway and possibly making the skin issue worse.[7]
Immune response
editCommensal S. epidermidis also influences the skin’s immune response. Through interacting with a host’s immune cells, the skin’s mucosal immune defense against various pathogens is strengthened. The skin commensal will directly interfere with harmful pathogens.[25]
In the case of S. aureus, S. epidermidis may amplify the innate immune response by causing a reaction of keratinocytes toward this pathogen.[7]
S. epidermidis produces molecules such as lipoteichoic acid (LTA), cell wall polysaccharides, peptidoglycan and aldehyde dipeptides which are recognized by toll-like receptors (TLRs) as molecules that modulate the immune response. These immunomodulatory molecules create a relationship between bacteria and keratinocytes and have a significant impact in the modulation of the innate immune response, mainly because of their interactions with TLRs.[7]
See also
editReferences
edit- ^ Schleifer KH, Kloos WE (January 1975). "Isolation and Characterization of Staphylococci from Human Skin I. Amended Descriptions of Staphylococcus epidermidis and Staphylococcus saprophyticus and Descriptions of Three New Species: Staphylococcus cohnii, Staphylococcus haemolyticus, and Staphylococcus xylosus". International Journal of Systematic Bacteriology. 25 (1): 50–61. doi:10.1099/00207713-25-1-50.
- ^ Fey PD, Olson ME (June 2010). "Current concepts in biofilm formation of Staphylococcus epidermidis". Future Microbiology. 5 (6): 917–933. doi:10.2217/fmb.10.56. PMC 2903046. PMID 20521936.
- ^ a b c d e f Paul SI, Rahman MM, Salam MA, Khan MA, Islam MT (2021-12-15). "Identification of marine sponge-associated bacteria of the Saint Martin's island of the Bay of Bengal emphasizing on the prevention of motile Aeromonas septicemia in Labeo rohita". Aquaculture. 545: 737156. doi:10.1016/j.aquaculture.2021.737156. ISSN 0044-8486.
- ^ a b Levinson W (2010). Review of Medical Microbiology and Immunology (11th ed.). pp. 94–99.
- ^ a b c d Salyers AA, Whitt DD (2002). Bacterial Pathogenesis: A Molecular Approach (2nd ed.). Washington, D.C.: ASM Press. ISBN 978-1-55581-171-6.
- ^ Queck SY, Otto M (2008). "Staphylococcus epidermidis and other Coagulase-Negative Staphylococci". Staphylococcus: Molecular Genetics. Caister Academic Press. ISBN 978-1-904455-29-5.
- ^ a b c d e Landemaine L, Da Costa G, Fissier E, Francis C, Morand S, Verbeke J, et al. (2023). "Staphylococcus epidermidis isolates from atopic or healthy skin have opposite effect on skin cells: potential implication of the AHR pathway modulation". Frontiers in Immunology. 14: 1098160. doi:10.3389/fimmu.2023.1098160. PMC 10250813. PMID 37304256.
- ^ "Staphylococcus epidermidis". VetBact.
- ^ Friedrich Julius Rosenbach at Who Named It?
- ^ "Todar's Online Textbook of Bacteriology: Staphylococcus aureus and Staphylococcal Disease". Kenneth Todar, PhD. Retrieved Dec 7, 2013.
- ^ "Bacteria Genomes – Staphylococcus epidermidis". Karyn's Genomes. EMBL-EBI. Archived from the original on 4 March 2010. Retrieved December 23, 2011.
- ^ dela Cruz TE, Torres JM (November 2012). "Gelatin Hydrolysis Test Protocol". American Society of Microbiology. Retrieved 2021-01-01.
- ^ Chabi R, Momtaz H (2019-12-05). "Virulence factors and antibiotic resistance properties of the Staphylococcus epidermidis strains isolated from hospital infections in Ahvaz, Iran". Tropical Medicine and Health. 47 (1): 56. doi:10.1186/s41182-019-0180-7. PMC 6896349. PMID 31844416.
- ^ Francois P, Schrenzel J (2008). "Rapid Diagnosis and Typing of Staphylococcus aureus". Staphylococcus: Molecular Genetics. Caister Academic Press. ISBN 978-1-904455-29-5.
- ^ Mackay IM, ed. (2007). Real-Time PCR in Microbiology: From Diagnosis to Characterization. Caister Academic Press. ISBN 978-1-904455-18-9.
- ^ Antunes AL, Secchi C, Reiter KC, Perez LR, de Freitas AL, D'Azevedo PA (January 2008). "Feasible identification of Staphylococcus epidermidis using desferrioxamine and fosfomycin disks". APMIS. 116 (1): 16–20. doi:10.1111/j.1600-0463.2008.00796.x. PMID 18254775. S2CID 205804740.
- ^ "Body Odor: Causes, Changes, Underlying Diseases & Treatment". Cleveland Clinic. Retrieved 2023-05-11.
- ^ a b Ara K, Hama M, Akiba S, Koike K, Okisaka K, Hagura T, et al. (April 2006). "Foot odor due to microbial metabolism and its control". Canadian Journal of Microbiology. 52 (4): 357–364. doi:10.1139/w05-130. PMID 16699586.
- ^ a b c Otto M (August 2009). "Staphylococcus epidermidis--the 'accidental' pathogen". Nature Reviews. Microbiology. 7 (8): 555–567. doi:10.1038/nrmicro2182. PMC 2807625. PMID 19609257.
- ^ Hedin G (1993). "Staphylococcus epidermidis--hospital epidemiology and the detection of methicillin resistance". Scandinavian Journal of Infectious Diseases. Supplementum. 90: 1–59. PMID 8303217.
- ^ Bek-Thomsen M, Lomholt HB, Kilian M (October 2008). "Acne is not associated with yet-uncultured bacteria". Journal of Clinical Microbiology. 46 (10): 3355–3360. doi:10.1128/JCM.00799-08. PMC 2566126. PMID 18716234.
- ^ Mustarichie R, Sulistyaningsih S, Runadi D (29 January 2020). "Antibacterial Activity Test of Extracts and Fractions of Cassava Leaves (Manihot esculenta Crantz) against Clinical Isolates of Staphylococcus epidermidis and Propionibacterium acnes Causing Acne". International Journal of Microbiology. 2020: 1975904. doi:10.1155/2020/1975904. PMC 7008253. PMID 32089694.
- ^ Kumar B, Pathak R, Mary PB, Jha D, Sardana K, Gautam HK (1 June 2016). "New insights into acne pathogenesis: Exploring the role of acne-associated microbial populations". Dermatologica Sinica. 34 (2): 67–73. doi:10.1016/j.dsi.2015.12.004.
- ^ Claudel JP, Auffret N, Leccia MT, Poli F, Corvec S, Dréno B (2019). "Staphylococcus epidermidis: A Potential New Player in the Physiopathology of Acne?". Dermatology. 235 (4): 287–294. doi:10.1159/000499858. PMID 31112983. S2CID 162170301.
- ^ a b Zheng Y, Hunt RL, Villaruz AE, Fisher EL, Liu R, Liu Q, et al. (March 2022). "Commensal Staphylococcus epidermidis contributes to skin barrier homeostasis by generating protective ceramides". Cell Host & Microbe. 30 (3): 301–313.e9. doi:10.1016/j.chom.2022.01.004. PMC 8917079. PMID 35123653.
Further reading
edit- Barros J, Grenho L, Manuel CM, Ferreira C, Melo L, Nunes OC, et al. (May 2014). "Influence of nanohydroxyapatite surface properties on Staphylococcus epidermidis biofilm formation". Journal of Biomaterials Applications. 28 (9): 1325–1335. doi:10.1177/0885328213507300. hdl:10216/103571. PMID 24122400. S2CID 37361193.
- Dong Y, Glaser K, Schlegel N, Claus H, Speer CP (November 2019). "An underestimated pathogen: Staphylococcus epidermidis induces pro-inflammatory responses in human alveolar epithelial cells". Cytokine. 123: 154761. doi:10.1016/j.cyto.2019.154761. PMID 31226437. S2CID 195260717.
- Feng G, Cheng Y, Worobo RW, Borca-Tasciuc DA, Moraru CI (October 2019). "Nanoporous anodic alumina reduces Staphylococcus biofilm formation". Letters in Applied Microbiology. 69 (4): 246–251. doi:10.1111/lam.13201. PMID 31357240.
- Gill SR, Fouts DE, Archer GL, Mongodin EF, Deboy RT, Ravel J, et al. (April 2005). "Insights on evolution of virulence and resistance from the complete genome analysis of an early methicillin-resistant Staphylococcus aureus strain and a biofilm-producing methicillin-resistant Staphylococcus epidermidis strain". Journal of Bacteriology. 187 (7): 2426–2438. doi:10.1128/JB.187.7.2426-2438.2005. PMC 1065214. PMID 15774886.
- Götz F (March 2002). "Staphylococcus and biofilms". Molecular Microbiology. 43 (6): 1367–1378. doi:10.1046/j.1365-2958.2002.02827.x. PMID 11952892. S2CID 10516046.
- Haidamak J, Davila Dos Santos G, Lima BJ, Soares VM, de Menezes RV, Bisson AA, et al. (September 2019). "Scalp microbiota alterations in children with pediculosis". Infection, Genetics and Evolution. 73: 322–331. doi:10.1016/j.meegid.2019.05.016. PMID 31121305.
- Izano EA, Amarante MA, Kher WB, Kaplan JB (January 2008). "Differential roles of poly-N-acetylglucosamine surface polysaccharide and extracellular DNA in Staphylococcus aureus and Staphylococcus epidermidis biofilms". Applied and Environmental Microbiology. 74 (2): 470–476. Bibcode:2008ApEnM..74..470I. doi:10.1128/AEM.02073-07. PMC 2223269. PMID 18039822.
- Méric G, Miragaia M, de Been M, Yahara K, Pascoe B, Mageiros L, et al. (April 2015). "Ecological Overlap and Horizontal Gene Transfer in Staphylococcus aureus and Staphylococcus epidermidis". Genome Biology and Evolution. 7 (5): 1313–1328. doi:10.1093/gbe/evv066. PMC 4453061. PMID 25888688.
- Nakatsuji T, Chen TH, Butcher AM, Trzoss LL, Nam SJ, Shirakawa KT, et al. (February 2018). "A commensal strain of Staphylococcus epidermidis protects against skin neoplasia". Science Advances. 4 (2): eaao4502. Bibcode:2018SciA....4.4502N. doi:10.1126/sciadv.aao4502. PMC 5834004. PMID 29507878.
- Otto M (August 2009). "Staphylococcus epidermidis--the 'accidental' pathogen". Nature Reviews. Microbiology. 7 (8): 555–567. doi:10.1038/nrmicro2182. PMC 2807625. PMID 19609257.
- Qin Z, Ou Y, Yang L, Zhu Y, Tolker-Nielsen T, Molin S, et al. (July 2007). "Role of autolysin-mediated DNA release in biofilm formation of Staphylococcus epidermidis". Microbiology. 153 (Pt 7): 2083–2092. doi:10.1099/mic.0.2007/006031-0. PMID 17600053.
- Schaeffer CR, Hoang TN, Sudbeck CM, Alawi M, Tolo IE, Robinson DA, et al. (5 October 2016). "Versatility of Biofilm Matrix Molecules in Staphylococcus epidermidis Clinical Isolates and Importance of Polysaccharide Intercellular Adhesin Expression during High Shear Stress". mSphere. 1 (5). doi:10.1128/mSphere.00165-16. PMC 5064449. PMID 27747298.
- Shahrooei M, Hira V, Khodaparast L, Khodaparast L, Stijlemans B, Kucharíková S, et al. (October 2012). "Vaccination with SesC decreases Staphylococcus epidermidis biofilm formation". Infection and Immunity. 80 (10): 3660–3668. doi:10.1128/IAI.00104-12. PMC 3457580. PMID 22802343.