The μ-opioid receptors (MOR) are a class of opioid receptors with a high affinity for enkephalins and beta-endorphin, but a low affinity for dynorphins. They are also referred to as μ(mu)-opioid peptide (MOP) receptors. The prototypical μ-opioid receptor agonist is morphine, the primary psychoactive alkaloid in opium and for which the receptor was named, with mu being the first letter of Morpheus, the compound's namesake in the original Greek. It is an inhibitory G-protein coupled receptor that activates the Gi alpha subunit, inhibiting adenylate cyclase activity, lowering cAMP levels.

Structure
editThe structure of the inactive μ-opioid receptor has been determined with the antagonists β-FNA[6] and alvimopan.[7] Many structures of the active state are also available, with agonists including DAMGO,[8] β-endorphin,[9] fentanyl and morphine.[10] The structure with the agonist BU72 has the highest resolution,[11] but contains unexplained features that may be experimental artifacts.[12][13] This large body of evidence has enabled structure-based design of a new class of opioids with functional selectivity.[14]
Splice variants
editThree variants of the μ-opioid receptor are well characterized, though reverse transcription polymerase chain reaction has identified up to 10 total splice variants in humans.[15][16][17]
| μ1 | More is known about the μ1 opioid receptor than the other variants. |
| μ2 | TRIMU 5 is a selective agonist of the μ2 receptor.[18] |
| μ3 | The μ3 variant was first described in 2003.[19] It is responsive to opiate alkaloids but not opioid peptides.[20] |
Location
editThey can exist either presynaptically or postsynaptically depending upon cell types.
The μ-opioid receptors exist mostly presynaptically in the periaqueductal gray region, and in the superficial dorsal horn of the spinal cord (specifically the substantia gelatinosa of Rolando). Other areas where they have been located include the external plexiform layer of the olfactory bulb, the nucleus accumbens, in several layers of the cerebral cortex, and in some of the nuclei of the amygdala, as well as the nucleus of the solitary tract.
Some MORs are also found in the intestinal tract. Activation of these receptors inhibits peristaltic action which causes constipation, a major side effect of μ agonists.[21]
Activation
editMOR can mediate acute changes in neuronal excitability via suppression of presynaptic release of GABA. Activation of the MOR leads to different effects on dendritic spines depending upon the agonist, and may be an example of functional selectivity at the μ-receptor.[22] The physiological and pathological roles of these two distinct mechanisms remain to be clarified. Perhaps, both might be involved in opioid addiction and opioid-induced deficits in cognition.
Activation of the μ-opioid receptor by an agonist such as morphine causes analgesia, sedation, slightly reduced blood pressure, itching, nausea, euphoria, decreased respiration, miosis (constricted pupils), and decreased bowel motility often leading to constipation. Some of these effects, such as analgesia, sedation, euphoria, itching and decreased respiration, tend to lessen with continued use as tolerance develops. Miosis and reduced bowel motility tend to persist; little tolerance develops to these effects.[citation needed]
The canonical MOR1 isoform is responsible for morphine-induced analgesia, whereas the alternatively spliced MOR1D isoform (through heterodimerization with the gastrin-releasing peptide receptor) is required for morphine-induced itching.[23]
Deactivation
editAs with other G protein-coupled receptors, signalling by the μ-opioid receptor is terminated through several different mechanisms, which are upregulated with chronic use, leading to rapid tachyphylaxis.[24] The most important regulatory proteins for the MOR are the β-arrestins arrestin beta 1 and arrestin beta 2,[25][26][27] and the RGS proteins RGS4, RGS9-2, RGS14, and RGSZ2.[28][29]
Long-term or high-dose use of opioids may also lead to additional mechanisms of tolerance becoming involved. This includes downregulation of MOR gene expression, so the number of receptors presented on the cell surface is actually reduced, as opposed to the more short-term desensitisation induced by β-arrestins or RGS proteins.[30][31][32] Another long-term adaptation to opioid use can be upregulation of glutamate and other pathways in the brain which can exert an opioid-opposing effect, so reduce the effects of opioid drugs by altering downstream pathways, regardless of MOR activation.[33][34]
Tolerance and overdoses
editFatal opioid overdose typically occurs due to bradypnea, hypoxemia, and decreased cardiac output (hypotension occurs due to vasodilation, and bradycardia further contributes to decreased cardiac output).[35][36][37] A potentiation effect occurs when opioids are combined with ethanol, benzodiazepines, barbiturates, or other central depressants which can result in rapid loss of consciousness and an increased risk of fatal overdose.[35][36]
Substantial tolerance to respiratory depression develops quickly, and tolerant individuals can withstand larger doses.[38] However, tolerance to respiratory depression is quickly lost during withdrawal and may be completely reversed within a week. Many overdoses occur in people who return to their previous dose after having lost their tolerance following cessation of opioids. This puts addicts who receive medical treatment for opioid addiction at great risk of overdose when they are released, as they may be particularly vulnerable to relapse.
Less commonly, massive overdoses have been known to cause circulatory collapse from vasodilation and bradycardia.[39]
Opioid overdoses can be rapidly reversed through the use of opioid antagonists, naloxone being the most widely used example.[35] Opioid antagonists work by binding competitively to μ-opioid receptors and displacing opioid agonists. Additional doses of naloxone may be necessary and supportive care should be given to prevent hypoxic brain injury by monitoring vital signs.
Tramadol and tapentadol carry additional risks associated with their dual effects as SNRIs and can cause serotonin syndrome and seizures. Despite these risks, there is evidence to suggest that these drugs have a lower risk of respiratory depression compared to morphine.[40]
Ligands
editAgonists
editEndogenous agonists
edit- Dynorphins (e.g., dynorphin A, dynorphin B)[41]
- Endomorphins (endomorphin-1, endomorphin-2)[41]
- Endorphins (e.g., β-endorphin)[41]
- Enkephalins (leu-enkephalin, met-enkephalin, adrenorphin)[41]
Full agonists
edit- Codeine[42]
- Fentanyl[42]
- Heroin[43]
- Hydrocodone[42]
- Hydromorphone[42]
- Levorphanol[42]
- Methadone[42][44]
- Morphine[42]
- Oxycodone[42]
- Oxymorphone[42]
- Pethidine (meperidine)[45][46]
- Tianeptine[47]
Partial agonists
edit- Buprenorphine[42]
- Butorphanol[44] (or antagonist)[48]
- Dezocine[49][50]
- Nalbuphine[44] (or antagonist)[48]
- Oliceridine[42]
- Pentazocine[42][44][46] (or antagonist)[48]
- Tramadol[43] (or partial agonist)[42]
Biased agonists
editPeripherally selective agonists
editIrreversible agonists
editAntagonists
editAntagonists and inverse agonists
edit- Cyclazocine[62]
- Cyprodime[63]
- Diprenorphine[64]
- Levallorphan[65]
- Nalmefene[66]
- Nalodeine[67]
- Nalorphine[65]
- Naloxone[68]
- Naltrexone[69]
- Samidorphan[70]
Note that some of the above drugs may actually be very weak partial agonists rather than silent antagonists.
Peripherally selective antagonists
edit- 6β-Naltrexol[71]
- Alvimopan[72]
- Axelopran[73]
- Bevenopran[74]
- Methylnaltrexone[75]
- Naldemedine[76]
- Naloxegol[77]
Gastrointestinally selective antagonists
edit- Naloxone (with oral administration)[78]
Irreversible antagonists
edit- β-Chlornaltrexamine[79][80]
- β-Funaltrexamine[81]
- Clocinnamox[82][83]
- Methocinnamox[84][85]
- Naloxazone[86]
- Naloxonazine[87]
Allosteric modulators
editPositive allosteric modulators
edit- BMS-986121[88][89]
- BMS‐986122[88][90][89][91]
- Comp5[92][93]
- Hydroxynorketamine (HNK)[94]
- Ignavine[95]
- Ketamine[94]
- MS1[88][96]
- Norketamine[94]
- Oxytocin[97][98][99]
Negative allosteric modulators
edit- Δ9-Tetrahydrocannabinol (THC) (weak)[88]
- Cannabidiol (weak)[88][89]
- Salvinorin A (weak)[88][89]
Silent allosteric modulators
editUnsorted allosteric modulators
edit- SCH-202676 (highly non-selective)[88][100]
See also
editReferences
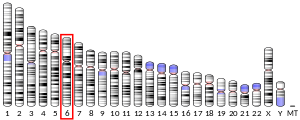
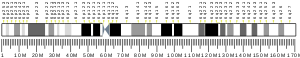
edit- ^ a b c GRCh38: Ensembl release 89: ENSG00000112038 – Ensembl, May 2017
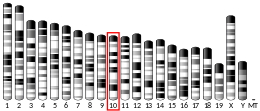
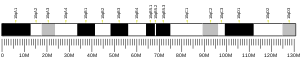
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000000766 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ Zhorov BS, Ananthanarayanan VS (March 2000). "Homology models of mu-opioid receptor with organic and inorganic cations at conserved aspartates in the second and third transmembrane domains". Archives of Biochemistry and Biophysics. 375 (1): 31–49. doi:10.1006/abbi.1999.1529. PMID 10683246.
- ^ Manglik A, Kruse AC, Kobilka TS, Thian FS, Mathiesen JM, Sunahara RK, et al. (March 2012). "Crystal structure of the μ-opioid receptor bound to a morphinan antagonist". Nature. 485 (7398): 321–326. Bibcode:2012Natur.485..321M. doi:10.1038/nature10954. PMC 3523197. PMID 22437502.
- ^ Robertson MJ, Papasergi-Scott MM, He F, Seven AB, Meyerowitz JG, Panova O, et al. (December 2022). "Structure determination of inactive-state GPCRs with a universal nanobody". Nature Structural & Molecular Biology. 29 (12): 1188–1195. doi:10.1038/s41594-022-00859-8. PMID 36396979.
- ^ Koehl A, Hu H, Maeda S, Zhang Y, Qu Q, Paggi JM, et al. (June 2018). "Structure of the μ-opioid receptor-Gi protein complex". Nature. 558 (7711): 547–552. Bibcode:2018Natur.558..547K. doi:10.1038/s41586-018-0219-7. PMC 6317904. PMID 29899455.
- ^ Wang Y, Zhuang Y, DiBerto JF, Zhou XE, Schmitz GP, Yuan Q, et al. (January 2023). "Structures of the entire human opioid receptor family". Cell. 186 (2): 413–427.e17. doi:10.1016/j.cell.2022.12.026. PMID 36638794. S2CID 255750597.
- ^ Zhuang Y, Wang Y, He B, He X, Zhou XE, Guo S, et al. (November 2022). "Molecular recognition of morphine and fentanyl by the human μ-opioid receptor". Cell. 185 (23): 4361–4375.e19. doi:10.1016/j.cell.2022.09.041. PMID 36368306. S2CID 253426623.
- ^ Huang W, Manglik A, Venkatakrishnan AJ, Laeremans T, Feinberg EN, Sanborn AL, et al. (August 2015). "Structural insights into μ-opioid receptor activation". Nature. 524 (7565): 315–321. Bibcode:2015Natur.524..315H. doi:10.1038/nature14886. PMC 4639397. PMID 26245379.
- ^ Zou R, Wang X, Li S, Chan HS, Vogel H, Yuan S (2022). "The role of metal ions in G protein-coupled receptor signalling and drug discovery". WIREs Computational Molecular Science. 12 (2): e1565. doi:10.1002/wcms.1565. ISSN 1759-0876. S2CID 237649760.
- ^ Munro TA (October 2023). "Reanalysis of a μ opioid receptor crystal structure reveals a covalent adduct with BU72". BMC Biology. 21 (1): 213. doi:10.1186/s12915-023-01689-w. PMC 10566028. PMID 37817141.
- ^ Faouzi A, Wang H, Zaidi SA, DiBerto JF, Che T, Qu Q, et al. (January 2023). "Structure-based design of bitopic ligands for the μ-opioid receptor". Nature. 613 (7945): 767–774. Bibcode:2023Natur.613..767F. doi:10.1038/s41586-022-05588-y. PMC 10328120. PMID 36450356.
- ^ Dortch-Carnes J, Russell K (January 2007). "Morphine-stimulated nitric oxide release in rabbit aqueous humor". Experimental Eye Research. 84 (1): 185–190. doi:10.1016/j.exer.2006.09.014. PMC 1766947. PMID 17094965.
- ^ Pan L, Xu J, Yu R, Xu MM, Pan YX, Pasternak GW (2005). "Identification and characterization of six new alternatively spliced variants of the human mu opioid receptor gene, Oprm". Neuroscience. 133 (1): 209–220. doi:10.1016/j.neuroscience.2004.12.033. PMID 15893644. S2CID 22410194.
- ^ Xu J, Lu Z, Narayan A, Le Rouzic VP, Xu M, Hunkele A, et al. (April 2017). "Alternatively spliced mu opioid receptor C termini impact the diverse actions of morphine". The Journal of Clinical Investigation. 127 (4): 1561–1573. doi:10.1172/JCI88760. PMC 5373896. PMID 28319053.
- ^ Eisenberg RM (April 1994). "TRIMU-5, a mu 2-opioid receptor agonist, stimulates the hypothalamo-pituitary-adrenal axis". Pharmacology, Biochemistry, and Behavior. 47 (4): 943–946. doi:10.1016/0091-3057(94)90300-X. PMID 8029266. S2CID 54354971.
- ^ Cadet P, Mantione KJ, Stefano GB (May 2003). "Molecular identification and functional expression of mu 3, a novel alternatively spliced variant of the human mu opiate receptor gene". Journal of Immunology. 170 (10): 5118–5123. doi:10.4049/jimmunol.170.10.5118. PMID 12734358.
- ^ Stefano GB (June 2004). "Endogenous morphine: a role in wellness medicine". Medical Science Monitor. 10 (6): ED5. PMID 15173675.
- ^ Chen W, Chung HH, Cheng JT (March 2012). "Opiate-induced constipation related to activation of small intestine opioid μ2-receptors". World Journal of Gastroenterology. 18 (12): 1391–1396. doi:10.3748/wjg.v18.i12.1391. PMC 3319967. PMID 22493554.
- ^ Liao D, Lin H, Law PY, Loh HH (February 2005). "Mu-opioid receptors modulate the stability of dendritic spines". Proceedings of the National Academy of Sciences of the United States of America. 102 (5): 1725–1730. Bibcode:2005PNAS..102.1725L. doi:10.1073/pnas.0406797102. JSTOR 3374498. PMC 545084. PMID 15659552.
- ^ Liu XY, Liu ZC, Sun YG, Ross M, Kim S, Tsai FF, et al. (October 2011). "Unidirectional cross-activation of GRPR by MOR1D uncouples itch and analgesia induced by opioids". Cell. 147 (2): 447–458. doi:10.1016/j.cell.2011.08.043. PMC 3197217. PMID 22000021.*Lay summary in: Dryden, J (October 13, 2011). "Researchers block morphine's itchy side effect". Washington University in St. Louis.
- ^ Martini L, Whistler JL (October 2007). "The role of mu opioid receptor desensitization and endocytosis in morphine tolerance and dependence". Current Opinion in Neurobiology. 17 (5): 556–564. doi:10.1016/j.conb.2007.10.004. PMID 18068348. S2CID 29491629.
- ^ Zuo Z (September 2005). "The role of opioid receptor internalization and beta-arrestins in the development of opioid tolerance". Anesthesia and Analgesia. 101 (3): 728–734. doi:10.1213/01.ANE.0000160588.32007.AD. PMID 16115983.
- ^ Marie N, Aguila B, Allouche S (November 2006). "Tracking the opioid receptors on the way of desensitization". Cellular Signalling. 18 (11): 1815–1833. doi:10.1016/j.cellsig.2006.03.015. PMID 16750901.
- ^ DuPen A, Shen D, Ersek M (September 2007). "Mechanisms of opioid-induced tolerance and hyperalgesia". Pain Management Nursing. 8 (3): 113–121. doi:10.1016/j.pmn.2007.02.004. PMID 17723928.
- ^ Garzón J, Rodríguez-Muñoz M, Sánchez-Blázquez P (May 2005). "Morphine alters the selective association between mu-opioid receptors and specific RGS proteins in mouse periaqueductal gray matter". Neuropharmacology. 48 (6): 853–868. doi:10.1016/j.neuropharm.2005.01.004. PMID 15829256. S2CID 23797166.
- ^ Hooks SB, Martemyanov K, Zachariou V (January 2008). "A role of RGS proteins in drug addiction". Biochemical Pharmacology. 75 (1): 76–84. doi:10.1016/j.bcp.2007.07.045. PMID 17880927.
- ^ Sirohi S, Dighe SV, Walker EA, Yoburn BC (November 2008). "The analgesic efficacy of fentanyl: relationship to tolerance and mu-opioid receptor regulation". Pharmacology, Biochemistry, and Behavior. 91 (1): 115–120. doi:10.1016/j.pbb.2008.06.019. PMC 2597555. PMID 18640146.
- ^ Lopez-Gimenez JF, Vilaró MT, Milligan G (November 2008). "Morphine desensitization, internalization, and down-regulation of the mu opioid receptor is facilitated by serotonin 5-hydroxytryptamine2A receptor coactivation". Molecular Pharmacology. 74 (5): 1278–1291. doi:10.1124/mol.108.048272. PMID 18703670. S2CID 6310244.
- ^ Kraus J (June 2009). "Regulation of mu-opioid receptors by cytokines". Frontiers in Bioscience. 1 (1): 164–170. doi:10.2741/e16. PMID 19482692.
- ^ García-Fuster MJ, Ramos-Miguel A, Rivero G, La Harpe R, Meana JJ, García-Sevilla JA (November 2008). "Regulation of the extrinsic and intrinsic apoptotic pathways in the prefrontal cortex of short- and long-term human opiate abusers". Neuroscience. 157 (1): 105–119. doi:10.1016/j.neuroscience.2008.09.002. PMID 18834930. S2CID 9022097.
- ^ Ueda H, Ueda M (June 2009). "Mechanisms underlying morphine analgesic tolerance and dependence". Frontiers in Bioscience. 14 (14): 5260–5272. doi:10.2741/3596. PMID 19482614.
- ^ a b c Blok (2017). "Opioid toxicity" (PDF). Clinical Key. Elsevier.
- ^ a b Hughes CG, McGrane S, Pandharipande PP (2012). "Sedation in the intensive care setting". Clinical Pharmacology. 4 (53): 53–63. doi:10.2147/CPAA.S26582. PMC 3508653. PMID 23204873.
- ^ Shanazari AA, Aslani Z, Ramshini E, Alaei H (2011). "Acute and chronic effects of morphine on cardiovascular system and the baroreflexes sensitivity during severe increase in blood pressure in rats". ARYA Atherosclerosis. 7 (3): 111–117. doi:10.1016/0277-9536(88)90399-1. PMC 3347855. PMID 22577457.
- ^ Algera MH, Olofsen E, Moss L, Dobbins RL, Niesters M, van Velzen M, et al. (March 2021). "Tolerance to Opioid-Induced Respiratory Depression in Chronic High-Dose Opioid Users: A Model-Based Comparison With Opioid-Naïve Individuals". Clinical Pharmacology and Therapeutics. 109 (3): 637–645. doi:10.1002/cpt.2027. PMC 7983936. PMID 32865832.
- ^ Krantz MJ, Palmer RB, Haigney MC (January 2021). "Cardiovascular Complications of Opioid Use: JACC State-of-the-Art Review". Journal of the American College of Cardiology. 77 (2): 205–223. doi:10.1016/j.jacc.2020.11.002. PMID 33446314. S2CID 231613932.
- ^ Houmes RJ, Voets MA, Verkaaik A, Erdmann W, Lachmann B (April 1992). "Efficacy and safety of tramadol versus morphine for moderate and severe postoperative pain with special regard to respiratory depression". Anesthesia and Analgesia. 74 (4): 510–514. doi:10.1213/00000539-199204000-00007. PMID 1554117. S2CID 24530179.
- ^ a b c d Tache S, Kerr PL, Sirbu C (2024). "The Foundational Science of Endogenous Opioids and Their Receptors". Endogenous Opioids. Advances in Neurobiology. Vol. 35. Cham: Springer International Publishing. pp. 9–26. doi:10.1007/978-3-031-45493-6_2. ISBN 978-3-031-45492-9. PMID 38874716.
- ^ a b c d e f g h i j k l m Gress K, Charipova K, Jung JW, Kaye AD, Paladini A, Varrassi G, et al. (September 2020). "A comprehensive review of partial opioid agonists for the treatment of chronic pain". Best Pract Res Clin Anaesthesiol. 34 (3): 449–461. doi:10.1016/j.bpa.2020.06.003. PMID 33004158.
- ^ a b Furlan AD, Murphy L (9 March 2022). "Opioids". Clinical Pain Management. Wiley. pp. 188–197. doi:10.1002/9781119701170.ch18. ISBN 978-1-119-70115-6.
- ^ a b c d Bidlack JM (2014). "Mixed Kappa/Mu Partial Opioid Agonists as Potential Treatments for Cocaine Dependence". Mixed κ/μ partial opioid agonists as potential treatments for cocaine dependence. Adv Pharmacol. Vol. 69. Elsevier. pp. 387–418. doi:10.1016/B978-0-12-420118-7.00010-X. ISBN 978-0-12-420118-7. PMID 24484983.
- ^ Bryant B, Knights K (2010). Pharmacology for Health Professionals (3rd ed.). Chatswood: Mosby Australia. ISBN 978-0-7295-3929-6.
- ^ a b Kelly E (August 2013). "Efficacy and ligand bias at the μ-opioid receptor". Br J Pharmacol. 169 (7): 1430–1446. doi:10.1111/bph.12222. PMC 3724102. PMID 23646826.
In some cases, agonists have such low efficacy that they cannot achieve the maximum response that a full agonist does, even when occupying all the receptors present in the tissue (Figure 1B); these agonists are called partial agonists. For example, with MOP receptors, ligands such as buprenorphine, meperidine and pentazocine behave as partial agonists in many cell signalling assays (McPherson et al., 2010).
- ^ Samuels BA, Nautiyal KM, Kruegel AC, Levinstein MR, Magalong VM, Gassaway MM, et al. (September 2017). "The Behavioral Effects of the Antidepressant Tianeptine Require the Mu-Opioid Receptor". Neuropsychopharmacology. 42 (10): 2052–2063. doi:10.1038/npp.2017.60. PMC 5561344. PMID 28303899.
- ^ a b c Hoskin PJ, Hanks GW (March 1991). "Opioid agonist-antagonist drugs in acute and chronic pain states". Drugs. 41 (3): 326–344. doi:10.2165/00003495-199141030-00002. PMID 1711441.
- ^ O'Brien JJ, Benfield P (August 1989). "Dezocine. A preliminary review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy". Drugs. 38 (2): 226–248. doi:10.2165/00003495-198938020-00005. PMID 2670517.
- ^ Ye RR, Jiang S, Xu X, Lu Y, Wang YJ, Liu JG (July 2022). "Dezocine as a potent analgesic: overview of its pharmacological characterization". Acta Pharmacol Sin. 43 (7): 1646–1657. doi:10.1038/s41401-021-00790-6. PMC 9253008. PMID 34737418.
- ^ a b c Azevedo Neto J, Costanzini A, De Giorgio R, Lambert DG, Ruzza C, Calò G (August 2020). "Biased versus Partial Agonism in the Search for Safer Opioid Analgesics". Molecules. 25 (17): 3870. doi:10.3390/molecules25173870. PMC 7504468. PMID 32854452.
- ^ Li X, He W, Chen Y, Yang G, Wan H, Zhang L, et al. (December 2017). "Discovery of SHR9352: A Highly Potent G Protein-Biased μ-Opioid Receptor Agonist". ACS Omega. 2 (12): 9261–9267. doi:10.1021/acsomega.7b01452. PMC 6645658. PMID 31457439.
- ^ Dhillon S (June 2024). "Tegileridine: First Approval". Drugs. 84 (6): 717–720. doi:10.1007/s40265-024-02033-4. PMID 38771484.
- ^ James IE, Skobieranda F, Soergel DG, Ramos KA, Ruff D, Fossler MJ (February 2020). "A First-in-Human Clinical Study With TRV734, an Orally Bioavailable G-Protein-Biased Ligand at the μ-Opioid Receptor". Clin Pharmacol Drug Dev. 9 (2): 256–266. doi:10.1002/cpdd.721. PMID 31286645.
- ^ Malinky CA, Lindsley CW, Han C (August 2021). "DARK Classics in Chemical Neuroscience: Loperamide". ACS Chem Neurosci. 12 (16): 2964–2973. doi:10.1021/acschemneuro.1c00382. PMID 34346690.
- ^ Vandenbossche J, Huisman M, Xu Y, Sanderson-Bongiovanni D, Soons P (April 2010). "Loperamide and P-glycoprotein inhibition: assessment of the clinical relevance". J Pharm Pharmacol. 62 (4): 401–412. doi:10.1211/jpp.62.04.0001. PMID 20604828.
- ^ Caruso TP, Takemori AE, Larson DL, Portoghese PS (April 1979). "Chloroxymorphamine, and opioid receptor site-directed alkylating agent having narcotic agonist activity". Science. 204 (4390): 316–318. doi:10.1126/science.86208. PMID 86208.
- ^ Caruso TP, Larson DL, Portoghese PS, Takemori AE (June 1980). "Pharmacological studies with an alkylating narcotic agonist, chloroxymorphamine, and antagonist, chlornaltrexamine". J Pharmacol Exp Ther. 213 (3): 539–544. PMID 6162947.
- ^ Woods JH, Lewis JW, Winger G, Butelman E, Broadbear J, Zernig G (1995). "Methoclocinnamox: A μ Partial Agonist With Pharmacotherapeutic Potential for Heroin Abuse". In National Institute on Drug Abuse (ed.). NIDA Research Monograph. DHEW publication. National Institute on Drug Abuse. pp. 195–219. Retrieved 9 August 2024.
- ^ Ling GS, Galetta S, Pasternak GW (March 1984). "Oxymorphazone: a long-acting opiate analgesic". Cell Mol Neurobiol. 4 (1): 1–13. doi:10.1007/BF00710938. PMID 6204757.
- ^ France CP, Jacobson AE, Woods JH (March 1984). "Irreversible and reversible narcotic agonists: discriminative and analgesic effects of buprenorphine, oxymorphazone, and morphine". NIDA Res Monogr. 49: 136–142. PMID 6207431.
- ^ Archer S, Glick SD, Bidlack JM (November 1996). "Cyclazocine revisited". Neurochem Res. 21 (11): 1369–1373. doi:10.1007/BF02532378. PMID 8947927.
- ^ Márki A, Monory K, Otvös F, Tóth G, Krassnig R, Schmidhammer H, et al. (October 1999). "Mu-opioid receptor specific antagonist cyprodime: characterization by in vitro radioligand and [35S]GTPgammaS binding assays". Eur J Pharmacol. 383 (2): 209–214. doi:10.1016/s0014-2999(99)00610-x. PMID 10585536.
- ^ Lewis JW, Husbands SM (2004). "The orvinols and related opioids--high affinity ligands with diverse efficacy profiles". Curr Pharm Des. 10 (7): 717–732. doi:10.2174/1381612043453027. PMID 15032698.
- ^ a b Dykstra LA (July 1990). "Butorphanol, levallorphan, nalbuphine and nalorphine as antagonists in the squirrel monkey". J Pharmacol Exp Ther. 254 (1): 245–252. PMID 2164093.
- ^ Green M, Veltri CA, Grundmann O (2024). "Nalmefene Hydrochloride: Potential Implications for Treating Alcohol and Opioid Use Disorder". Subst Abuse Rehabil. 15: 43–57. doi:10.2147/SAR.S431270. PMC 10999209. PMID 38585160.
- ^ Martin WR (17 April 2013). "The Evolution of Concepts of Opioid Receptors". In Pasternak G (ed.). The Opiate Receptors. Springer Science & Business Media. pp. 4–. ISBN 978-1-60761-990-1.
- ^ Saari TI, Strang J, Dale O (April 2024). "Clinical Pharmacokinetics and Pharmacodynamics of Naloxone". Clin Pharmacokinet. 63 (4): 397–422. doi:10.1007/s40262-024-01355-6. PMC 11052794. PMID 38485851.
- ^ Sudakin D (March 2016). "Naltrexone: Not Just for Opioids Anymore". J Med Toxicol. 12 (1): 71–75. doi:10.1007/s13181-015-0512-x. PMC 4781804. PMID 26546222.
- ^ Chaudhary AM, Khan MF, Dhillon SS, Naveed S (July 2019). "A Review of Samidorphan: A Novel Opioid Antagonist". Cureus. 11 (7): e5139. doi:10.7759/cureus.5139. PMC 6741386. PMID 31523568.
- ^ Yancey-Wrona J, Dallaire B, Bilsky E, Bath B, Burkart J, Webster L, et al. (December 2011). "6β-naltrexol, a peripherally selective opioid antagonist that inhibits morphine-induced slowing of gastrointestinal transit: an exploratory study". Pain Med. 12 (12): 1727–1737. doi:10.1111/j.1526-4637.2011.01279.x. PMID 22123184.
- ^ Camilleri M (April 2005). "Alvimopan, a selective peripherally acting mu-opioid antagonist". Neurogastroenterol Motil. 17 (2): 157–165. doi:10.1111/j.1365-2982.2005.00640.x. PMID 15787936.
- ^ Long DD, Armstrong SR, Beattie DT, Campbell CB, Church TJ, Colson PJ, et al. (December 2019). "Discovery of Axelopran (TD-1211): A Peripherally Restricted μ-Opioid Receptor Antagonist". ACS Med Chem Lett. 10 (12): 1641–1647. doi:10.1021/acsmedchemlett.9b00406. PMC 6912869. PMID 31857840.
- ^ Pannemans J, Vanuytsel T, Tack J (October 2018). "New developments in the treatment of opioid-induced gastrointestinal symptoms". United European Gastroenterol J. 6 (8): 1126–1135. doi:10.1177/2050640618796748. PMC 6169055. PMID 30288274.
- ^ Yuan CS, Israel RJ (May 2006). "Methylnaltrexone, a novel peripheral opioid receptor antagonist for the treatment of opioid side effects". Expert Opin Investig Drugs. 15 (5): 541–552. doi:10.1517/13543784.15.5.541. PMID 16634692.
- ^ Stern EK, Brenner DM (2018). "Spotlight on naldemedine in the treatment of opioid-induced constipation in adult patients with chronic noncancer pain: design, development, and place in therapy". J Pain Res. 11: 195–199. doi:10.2147/JPR.S141322. PMC 5774487. PMID 29391826.
- ^ Corsetti M, Tack J (August 2015). "Naloxegol: the first orally administered, peripherally acting, mu opioid receptor antagonist, approved for the treatment of opioid-induced constipation". Drugs Today (Barc). 51 (8): 479–489. doi:10.1358/dot.2015.51.8.2364896. PMID 26380386.
- ^ Leppert W (January 2014). "Oxycodone/naloxone in the management of patients with pain and opioid-induced bowel dysfunction". Curr Drug Targets. 15 (1): 124–135. doi:10.2174/13894501113149990210. PMID 24020972.
- ^ Portoghese PS, Larson DL, Jiang JB, Takemori AE, Caruso TP (July 1978). "6beta-[N,N-Bis(2-chloroethyl)amino]-17-(cyclopropylmethyl)-4,5alpha-epoxy-3,14-dihydroxymorphinan(chlornaltrexamine) a potent opioid receptor alkylating agent with ultralong narcotic antagonist actitivty". J Med Chem. 21 (7): 598–599. doi:10.1021/jm00205a002. PMID 209185.
- ^ Portoghese PS, Larson DL, Jiang JB, Caruso TP, Takemori AE (February 1979). "Synthesis and pharmacologic characterization of an alkylating analogue (chlornaltrexamine) of naltrexone with ultralong-lasting narcotic antagonist properties". J Med Chem. 22 (2): 168–173. doi:10.1021/jm00188a008. PMID 218009.
- ^ Ward SJ, Portoghese PS, Takemori AE (March 1982). "Pharmacological characterization in vivo of the novel opiate, beta-funaltrexamine". J Pharmacol Exp Ther. 220 (3): 494–498. PMID 6121045.
- ^ Comer SD, Burke TF, Lewis JW, Woods JH (September 1992). "Clocinnamox: a novel, systemically-active, irreversible opioid antagonist". J Pharmacol Exp Ther. 262 (3): 1051–1056. PMID 1326622.
- ^ Burke TF, Woods JH, Lewis JW, Medzihradsky F (November 1994). "Irreversible opioid antagonist effects of clocinnamox on opioid analgesia and mu receptor binding in mice". J Pharmacol Exp Ther. 271 (2): 715–721. PMID 7965787.
- ^ Jordan CG, Kennalley AL, Roberts AL, Nemes KM, Dolma T, Piper BJ (April 2022). "The Potential of Methocinnamox as a Future Treatment for Opioid Use Disorder: A Narrative Review". Pharmacy. 10 (3): 48. doi:10.3390/pharmacy10030048. PMC 9149874. PMID 35645327.
- ^ Broadbear JH, Sumpter TL, Burke TF, Husbands SM, Lewis JW, Woods JH, et al. (September 2000). "Methocinnamox is a potent, long-lasting, and selective antagonist of morphine-mediated antinociception in the mouse: comparison with clocinnamox, beta-funaltrexamine, and beta-chlornaltrexamine". J Pharmacol Exp Ther. 294 (3): 933–940. PMID 10945843.
- ^ Pasternak GW, Childers SR, Snyder SH (September 1980). "Naloxazone, a long-acting opiate antagonist: effects on analgesia in intact animals and on opiate receptor binding in vitro". J Pharmacol Exp Ther. 214 (3): 455–462. PMID 6105201.
- ^ Hahn EF, Pasternak GW (1982). "Naloxonazine, a potent, long-lasting inhibitor of opiate binding sites". Life Sci. 31 (12–13): 1385–1388. doi:10.1016/0024-3205(82)90387-3. PMID 6292633.
- ^ a b c d e f g h Livingston KE, Traynor JR (July 2018). "Allostery at opioid receptors: modulation with small molecule ligands". Br J Pharmacol. 175 (14): 2846–2856. doi:10.1111/bph.13823. PMC 6016636. PMID 28419415.
- ^ a b c d Burford NT, Traynor JR, Alt A (January 2015). "Positive allosteric modulators of the μ-opioid receptor: a novel approach for future pain medications". Br J Pharmacol. 172 (2): 277–286. doi:10.1111/bph.12599. PMC 4292945. PMID 24460691.
- ^ Zhu L, Cui Z, Zhu Q, Zha X, Xu Y (2018). "Novel Opioid Receptor Agonists with Reduced Morphine-like Side Effects". Mini Rev Med Chem. 18 (19): 1603–1610. doi:10.2174/1389557518666180716124336. PMID 30009707.
- ^ Kandasamy R, Hillhouse TM, Livingston KE, Kochan KE, Meurice C, Eans SO, et al. (April 2021). "Positive allosteric modulation of the mu-opioid receptor produces analgesia with reduced side effects". Proc Natl Acad Sci U S A. 118 (16). doi:10.1073/pnas.2000017118. PMC 8072371. PMID 33846240.
- ^ González AM, Jubete AG (April 2024). "Dualism, allosteric modulation, and biased signaling of opioid receptors: Future therapeutic potential". Rev Esp Anestesiol Reanim (Engl Ed). 71 (4): 298–303. doi:10.1016/j.redare.2022.06.009. PMID 37683976.
- ^ Pryce KD, Kang HJ, Sakloth F, Liu Y, Khan S, Toth K, et al. (September 2021). "A promising chemical series of positive allosteric modulators of the μ-opioid receptor that enhance the antinociceptive efficacy of opioids but not their adverse effects". Neuropharmacology. 195: 108673. doi:10.1016/j.neuropharm.2021.108673. PMC 8410669. PMID 34153316.
- ^ a b c Gomes I, Gupta A, Margolis EB, Fricker LD, Devi LA (August 2024). "Ketamine and major ketamine metabolites function as allosteric modulators of opioid receptors". Mol Pharmacol. 106 (5): 240–252. doi:10.1124/molpharm.124.000947. PMC 11493337. PMID 39187388.
- ^ Hovah ME, Holzgrabe U (May 2024). "Bivalent and bitopic ligands of the opioid receptors: The prospects of a dual approach". Med Res Rev. 44 (6): 2545–2599. doi:10.1002/med.22050. PMID 38751227.
- ^ Bisignano P, Burford NT, Shang Y, Marlow B, Livingston KE, Fenton AM, et al. (September 2015). "Ligand-Based Discovery of a New Scaffold for Allosteric Modulation of the μ-Opioid Receptor". J Chem Inf Model. 55 (9): 1836–43. doi:10.1021/acs.jcim.5b00388. PMC 4703110. PMID 26347990.
- ^ Meguro Y, Miyano K, Hirayama S, Yoshida Y, Ishibashi N, Ogino T, et al. (May 2018). "Neuropeptide oxytocin enhances μ opioid receptor signaling as a positive allosteric modulator". J Pharmacol Sci. 137 (1): 67–75. doi:10.1016/j.jphs.2018.04.002. PMID 29716811.
- ^ Miyano K, Yoshida Y, Hirayama S, Takahashi H, Ono H, Meguro Y, et al. (October 2021). "Oxytocin Is a Positive Allosteric Modulator of κ-Opioid Receptors but Not δ-Opioid Receptors in the G Protein Signaling Pathway". Cells. 10 (10): 2651. doi:10.3390/cells10102651. PMC 8534029. PMID 34685631.
- ^ Mizuguchi T, Miyano K, Yamauchi R, Yoshida Y, Takahashi H, Yamazaki A, et al. (January 2023). "The first structure-activity relationship study of oxytocin as a positive allosteric modulator for the µ opioid receptor". Peptides. 159: 170901. doi:10.1016/j.peptides.2022.170901. PMID 36347314.
- ^ Fawzi AB, Macdonald D, Benbow LL, Smith-Torhan A, Zhang H, Weig BC, et al. (January 2001). "SCH-202676: An allosteric modulator of both agonist and antagonist binding to G protein-coupled receptors". Mol Pharmacol. 59 (1): 30–37. doi:10.1124/mol.59.1.30. PMID 11125021.
External links
edit- "Opioid Receptors: μ". IUPHAR Database of Receptors and Ion Channels. International Union of Basic and Clinical Pharmacology.
- mu+Opioid+Receptor at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Human OPRM1 genome location and OPRM1 gene details page in the UCSC Genome Browser.