The peritoneum is the serous membrane forming the lining of the abdominal cavity or coelom in amniotes and some invertebrates, such as annelids. It covers most of the intra-abdominal (or coelomic) organs, and is composed of a layer of mesothelium supported by a thin layer of connective tissue. This peritoneal lining of the cavity supports many of the abdominal organs and serves as a conduit for their blood vessels, lymphatic vessels, and nerves.
| Peritoneum | |
|---|---|
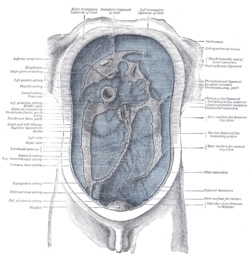 The peritoneum, colored in blue | |
 | |
| Details | |
| Pronunciation | /ˌpɛrɪtəˈniːəm/ |
| Part of | Abdomen |
| Identifiers | |
| Latin | peritoneum |
| MeSH | D010537 |
| TA98 | A10.1.02.002 A10.1.02.005 A10.1.02.006 |
| TA2 | 3729 |
| TH | H3.04.08.0.00001 |
| FMA | 9584 |
| Anatomical terminology | |
The abdominal cavity (the space bounded by the vertebrae, abdominal muscles, diaphragm, and pelvic floor) is different from the intraperitoneal space (located within the abdominal cavity but wrapped in peritoneum). The structures within the intraperitoneal space are called "intraperitoneal" (e.g., the stomach and intestines), the structures in the abdominal cavity that are located behind the intraperitoneal space are called "retroperitoneal" (e.g., the kidneys), and those structures below the intraperitoneal space are called "subperitoneal" or "infraperitoneal" (e.g., the bladder).
Structure
editLayers
editThe peritoneum is one continuous sheet, forming two layers and a potential space between them: the peritoneal cavity.
The outer layer, the parietal peritoneum, is attached to the abdominal wall and the pelvic walls.[1] The tunica vaginalis, the serous membrane covering the male testis, is derived from the vaginal process, an outpouching of the parietal peritoneum.
The inner layer, the visceral peritoneum, is wrapped around the visceral organs, located inside the intraperitoneal space for protection. It is thinner than the parietal peritoneum. The mesentery is a double layer of visceral peritoneum that attaches to the gastrointestinal tract. There are often blood vessels, nerves, and other structures between these layers. The space between these two layers is technically outside of the peritoneal sac, and thus not in the peritoneal cavity.
The potential space between these two layers is the peritoneal cavity, filled with a small amount (about 50 mL) of slippery serous fluid that allows the two layers to slide freely over each other.
The right paracolic gutter is continuous with the right and left subhepatic spaces. The epiploic foramen allows communication between the greater sac and the lesser sac.[2] The peritoneal space in males is closed, while the peritoneal space in females is continuous with the extraperitoneal pelvis through openings of the fallopian tubes, the uterus, and the vagina.[3]
Subdivisions
editPeritoneal folds are omentums, mesenteries and ligaments; they connect organs to each other or to the abdominal wall.[4] There are two main regions of the peritoneal cavity, connected by the omental foramen.
- The greater sac, represented in red in the diagrams above.
- The lesser sac, represented in blue. The lesser sac is divided into two "omenta":
- The lesser omentum (or hepatogastric) is attached to the lesser curvature of the stomach and the liver.[5]
- The greater omentum (or gastrocolic) hangs from the greater curvature of the stomach and loops down in front of the intestines before curving back upwards to attach to the transverse colon.[5] In effect it is draped in front of the intestines like an apron and may serve as an insulating or protective layer.[5]
The mesentery is the part of the peritoneum through which most abdominal organs are attached to the abdominal wall and supplied with blood and lymph vessels and nerves.
| Sources | Structure | From | To | Contains |
| Dorsal mesentery | Greater omentum | Greater curvature of stomach (and spleen) | Transverse colon | right and left gastroepiploic vessels and fat |
| Gastrosplenic ligament | Stomach | Spleen | Short gastric artery, Left gastroepiploic artery | |
| Gastrophrenic ligament | Stomach | Diaphragm | Left inferior phrenic artery | |
| Gastrocolic ligament | Stomach | Transverse colon | Right gastroepiploic artery | |
| Splenorenal ligament | Spleen | Kidney | Splenic artery, Tail of pancreas | |
| Ventral mesentery | Lesser omentum | Lesser curvature of the stomach (and duodenum) | Liver | The right free margin-hepatic artery, portal vein, and bile duct,lymph nodes and the lymph vessels,hepatic plexus of nerve,all enclosed in perivascular fibrous sheath. Along the lesser curvature of the stomach-left and right gastric artery,gastric group of lymph nodes and lyphatics, branches from gastric nerve. |
| Hepatogastric ligament | Stomach | Liver | Right and left gastric artery | |
| Hepatoduodenal ligament | Duodenum | Liver | Hepatic artery proper, hepatic portal vein, bile duct, autonomic nerves |
| Sources | Structure | From | To | Contains |
| Dorsal mesentery | Mesentery proper | Small intestine (jejunum and ileum) | Posterior abdominal wall | Superior mesenteric artery, accompanying veins, autonomic nerve plexuses, lymphatics, 100–200 lymph nodes and connective tissue with fat |
| Transverse mesocolon | Transverse colon | Posterior abdominal wall | Middle colic | |
| Sigmoid mesocolon | Sigmoid colon | Pelvic wall | Sigmoid arteries and superior rectal artery | |
| Mesoappendix | Mesentery of ileum | Appendix | Appendicular artery |
Other ligaments and folds
edit| Sources | Structure | From | To | Contains |
| Ventral mesentery | Falciform ligament | Liver | Thoracic diaphragm, anterior abdominal wall | Round ligament of liver, paraumbilical vein |
| Left umbilical vein | Round ligament of liver | Liver | Umbilicus | |
| Ventral mesentery | Coronary ligament | Liver | Thoracic diaphragm | |
| Ductus venosus | Ligamentum venosum | Liver | Liver | |
| Phrenicocolic ligament | Left colic flexure | Thoracic diaphragm | ||
| Ventral mesentery | Left triangular ligament, right triangular ligament | Liver | ||
| Umbilical folds | Urinary bladder | |||
| Ileocecal fold | Ileum | Cecum | ||
| Broad ligament of the uterus | Uterus | Pelvic wall | Mesovarium, mesosalpinx, mesometrium | |
| Round ligament of uterus | Uterus | Inguinal canal | ||
| Suspensory ligament of the ovary | Ovary | Pelvic wall | Ovarian artery |
In addition, in the pelvic cavity there are several structures that are usually named not for the peritoneum, but for the areas defined by the peritoneal folds:
| Name | Location | Sexes possessing structure |
| Rectovesical pouch | Between rectum and urinary bladder | Male only |
| Rectouterine pouch | Between rectum and uterus | Female only |
| Vesicouterine pouch | Between urinary bladder and uterus | Female only |
| Pararectal fossa | Surrounding rectum | Male and female |
| Paravesical fossa | Surrounding urinary bladder | Male and female |
Classification of abdominal structures
editThe structures in the abdomen are classified as intraperitoneal, mesoperitoneal, retroperitoneal or infraperitoneal depending on whether they are covered with visceral peritoneum and whether they are attached by mesenteries (mensentery, mesocolon).
| Intraperitoneal | Mesoperitoneal | Retroperitoneal ( or Extraperitoneal ) | Infraperitoneal / Subperitoneal |
| Stomach, half of the first part of the duodenum [2.2 cm], jejunum, ileum, cecum, appendix, transverse colon, sigmoid colon, rectum (upper 1/3) | The rest of the duodenum, ascending colon, descending colon, rectum (middle 1/3) | Rectum (lower 1/3) | |
| Spleen, pancreas (only tail) | Liver | Pancreas (except tail) | |
| Kidneys, adrenal glands, proximal ureters, renal vessels | Urinary bladder, distal ureters | ||
| In women: ovaries | Gonadal blood vessels, Uterus, Fallopian Tubes | ||
| Inferior vena cava, aorta |
Structures that are intraperitoneal are generally mobile, while those that are retroperitoneal are relatively fixed in their location.
Some structures, such as the kidneys, are "primarily retroperitoneal", while others such as the majority of the duodenum, are "secondarily retroperitoneal", meaning that structure developed intraperitoneally but lost its mesentery and thus became retroperitoneal.
Development
editThe peritoneum develops ultimately from the mesoderm of the trilaminar embryo. As the mesoderm differentiates, one region known as the lateral plate mesoderm splits to form two layers separated by an intraembryonic coelom. These two layers develop later into the visceral and parietal layers found in all serous cavities, including the peritoneum.
As an embryo develops, the various abdominal organs grow into the abdominal cavity from structures in the abdominal wall. In this process they become enveloped in a layer of peritoneum. The growing organs "take their blood vessels with them" from the abdominal wall, and these blood vessels become covered by peritoneum, forming a mesentery.[6]
Peritoneal folds develop from the ventral and dorsal mesentery of the embryo.[4]
Clinical significance
editImaging assessment
editCT scan is a fast (15 seconds) and efficient way in visualising the peritoneal spaces. Although ultrasound is good at visualizing peritoneal collections and ascites, without ionising radiation, it does not provide a good overall assessment of all the peritoneal cavities. MRI scan is also increasingly used to visualise peritoneal diseases, but requires long scan time (30 to 45 minutes) and prone to motion artifacts due to respiration and peristalsis and chemical shift artifacts at the bowel-mesentery interface. Those with peritoneal carcinomatosis, acute pancreatitis, and intraabdominal sepsis may not tolerate prolonged MRI scan.[3]
Peritoneal dialysis
editIn one form of dialysis, called peritoneal dialysis, a glucose solution is sent through a tube into the peritoneal cavity. The fluid is left there for a prescribed amount of time to absorb waste products, and then removed through the tube. The reason for this effect is the high number of arteries and veins in the peritoneal cavity. Through the mechanism of diffusion, waste products are removed from the blood.
Peritonitis
editPeritonitis is the inflammation of the peritoneum. It is more commonly associated to infection from a punctured organ of the abdominal cavity. It can also be provoked by the presence of fluids that produce chemical irritation, such as gastric acid or pancreatic juice. Peritonitis causes fever, tenderness, and pain in the abdominal area, which can be localized or diffuse. The treatment involves rehydration, administration of antibiotics, and surgical correction of the underlying cause. Mortality is higher in the elderly and if present for a prolonged time.[7]
Primary peritoneal carcinoma
editPrimary peritoneal cancer is a cancer of the cells lining the peritoneum.
Etymology
edit"Peritoneum" is derived from Greek: περιτόναιον, romanized: peritonaion, lit. 'peritoneum, abdominal membrane'[8] via Latin. In Greek, περί, peri means "around", while τείνω, teino means "to stretch"; thus, "peritoneum" means "stretched over".[8]
Additional images
edit-
Median sagittal section of pelvis, showing the arrangement of fasciæ
-
Horizontal disposition of the peritoneum in the lower part of the abdomen
-
Sagittal section through posterior abdominal wall, showing the relations of the capsule of the kidney
-
Topography of thoracic and abdominal viscera
-
Horizontal disposition of the peritoneum in the upper part of the abdomen
-
Cytology of the normal mesothelial cells that line the peritoneum, with typical features.[9] Wright's stain
See also
editReferences
edit- ^ Tank PW (2013). "Chapter 4: The abdomen". Grant's dissector (Fifteenth ed.). Philadelphia. ISBN 978-1-60913-606-2.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Jones, J. (14 April 2009). Epiploic Foramen | Radiopaedia.org. Radiopaedia. doi:10.53347/rID-6059. Retrieved 21 May 2022.
- ^ a b Tirkes, Temel; Sandrasegaran, Kumaresan; Patel, Aashish A.; Hollar, Margaret A.; Tejada, Juan G.; Tann, Mark; Akisik, Fatih M.; Lappas, John C. (March 2012). "Peritoneal and Retroperitoneal Anatomy and Its Relevance for Cross-Sectional Imaging". RadioGraphics. 32 (2): 437–451. doi:10.1148/rg.322115032. ISSN 0271-5333. PMID 22411941.
- ^ a b Drake, R. L.; Vogl, A.W.; Mitchell, A.W. (4 April 2009). "Abdominal Viscera". Gray's Anatomy for Students. Philadelphia, PA: Elsevier Health Sciences. p. 295. ISBN 9781437720556. OCLC 489070574.
- ^ a b c Tortora GJ, Anagnostakos NP (1984). Principles of anatomy and physiology (4th ed.). New York: Harper & Row. ISBN 978-0-06-046656-5.
- ^ "Peritoneum" (PDF). healthoracle.org. Archived from the original (PDF) on 23 April 2016. Retrieved 14 April 2018.
- ^ Longo D, Fauci A, Kasper D, Hauser S, Jameson J, Loscalzo J (2012). Harrison's Principles of Internal Medicine (18th ed.). New York: McGraw-Hill. pp. 2518–2519. ISBN 978-0-07-174889-6.
- ^ a b "Peritoneum - Origin and meaning of peritoneum by Online Etymology Dictionary". www.etymonline.com. Retrieved 14 April 2018.
- ^ Image by Mikael Häggström, MD. Sources for mentioned features:
- "Mesothelial cytopathology". Libre Pathology. Retrieved 2022-10-18.
- Shidham VB, Layfield LJ (2021). "Introduction to the second edition of 'Diagnostic Cytopathology of Serous Fluids' as CytoJournal Monograph (CMAS) in Open Access". CytoJournal. 18: 30. doi:10.25259/CMAS_02_01_2021. PMC 8813611. PMID 35126608.