An itch (also known as pruritus) is a sensation that causes a strong desire or reflex to scratch.[1] Itches have resisted many attempts to be classified as any one type of sensory experience. Itches have many similarities to pain, and while both are unpleasant sensory experiences, their behavioral response patterns are different. Pain creates a withdrawal reflex, whereas itches leads to a scratch reflex.[2]
| Itch | |
|---|---|
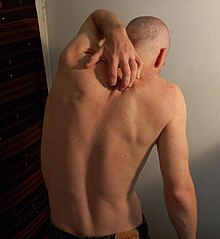 | |
| A man scratching his back | |
| Specialty | Dermatology |
| Symptoms | Compulsion to scratch an irritated area of skin |
| Causes | Certain infections, allergies, blood derangements and environmental factors |
| Risk factors | Dry skin |
| Diagnostic method | Often based on the causes of itching |
| Differential diagnosis | Pain |
| Treatment | Antipruritics, phototherapy |
Unmyelinated nerve fibers for itches and pain both originate in the skin. Information for them is conveyed centrally in two distinct systems that both use the same nerve bundle and spinothalamic tract.[3]
Classification
editMost commonly, an itch is felt in one place. If it is felt all over the body, then it is called generalized itch or generalized pruritus.[4] Generalized itch is infrequently a symptom of a serious underlying condition, such as cholestatic liver disease.
If the sensation of itching persists for six weeks or longer, then it is called chronic itch or chronic pruritus.[4][5] Chronic idiopathic pruritus or Chronic Pruritus of Unknown Origin is a form of itch that persists for longer than six weeks, and for which no clear cause can be identified.[6][7]
Signs and symptoms
editPain and itch have very different behavioral response patterns. Pain elicits a withdrawal reflex, which leads to retraction and therefore a reaction trying to protect an endangered part of the body. Itch in contrast creates a scratch reflex, which draws one to the affected skin site. Itch generates stimulus of a foreign object underneath or upon the skin and also the urge to remove it. For example, responding to a local itch sensation is an effective way to remove insects from one's skin.
Scratching has traditionally been regarded as a way to relieve oneself by reducing the annoying itch sensation. However, there are hedonic aspects to scratching, as one would find noxious scratching highly pleasurable.[2] This can be problematic with chronic itch patients, such as ones with atopic dermatitis, who may scratch affected spots until they no longer produce a pleasant or painful sensation, instead of when the itch sensation disappears.[8] It has been hypothesized that motivational aspects of scratching include the frontal brain areas of reward and decision making. These aspects might therefore contribute to the compulsive nature of itch and scratching.[2]
Contagious itch
editEvents of "contagious itch" are very common occurrences. Even a discussion on the topic of itch can give one the desire to scratch. Itch is likely to be more than a localized phenomenon in the place one scratches. Results from a study showed that itching and scratching were induced purely by visual stimuli in a public lecture on itching.[9] The sensation of pain can also be induced in a similar fashion, often by listening to a description of an injury, or viewing an injury itself.
There is little detailed data on central activation for contagious itching, but it is hypothesized that a human mirror neuron system exists in which one imitates certain motor actions when they view others performing the same action. A similar hypothesis has been used to explain the cause of contagious yawning.[2]
Itch inhibition due to pain
editStudies done in the last decade have shown that itch can be inhibited by many other forms of painful stimuli, such as noxious heat,[10] physical rubbing/scratching, noxious chemicals, and electric shock.[11]
Causes
editInfectious
edit- Body louse, found in substandard living conditions
- Cutaneous larva migrans, a skin disease caused by hookworm infection
- Head lice, if limited to the neck and scalp
- Herpes, a viral disease
- Insect bites, such as those from mosquitos or chiggers
- Pubic lice, if limited to the genital area
- Scabies, especially when several other persons in close contact also itch
- Shaving, which may irritate the skin
- Swimmer's itch, a short-term immune reaction
- Varicella – i.e. chickenpox, prevalent among young children and highly contagious
- Tungiasis, ectoparasite of skin
Environmental and allergic
edit- Allergic reaction to contact with specific chemicals, such as urushiol, derived from poison ivy or poison oak, or Balsam of Peru, found in many foods and fragrances.[12][13] Certain allergens may be diagnosed in a patch test.[14][15]
- Foreign objects on the skin are the most common cause of non-pathological itching.
- Photodermatitis – sunlight reacts with chemicals in the skin, leading to the formation of irritant metabolites.
- Urticaria (also called hives) usually causes itching.
Dermatologic
edit- Dandruff, an unusually large amount of flaking is associated with this sensation.
- Punctate palmoplantar keratoderma, a group of disorders characterized by abnormal thickening of the palms and soles.
- Skin conditions (such as psoriasis, eczema, seborrhoeic dermatitis, sunburn, athlete's foot, and hidradenitis suppurativa). Most are of an inflammatory nature.
- Scab healing, scar growth, and the development or emergence of moles, pimples, and ingrown hairs from below the epidermis.
- Xerosis, dry skin, frequently seen in the winter and also associated with older age, frequent bathing in hot showers or baths, and high-temperature and low-humidity environments.
Other diseases
edit- Diabetes mellitus, a group of metabolic diseases in which a person has high blood sugar
- Hyperparathyroidism, overactivity of the parathyroid glands resulting in excess production of parathyroid hormone (PTH)[16]
- Iron deficiency anemia, a common anemia (low red blood cell or hemoglobin levels)
- Cholestasis, where bile acids leaking into the serum activate peripheral opioid receptors, resulting in the characteristic generalized, severe itching
- Malignancy or internal cancer, such as lymphoma or Hodgkin's disease[17]
- Polycythemia, which can cause generalized itching due to increased histamines
- Psychiatric disease ("psychogenic itch", as may be seen in delusional parasitosis)
- Thyroid illness
- Uraemia – the itching sensation this causes is known as uremic pruritus
Medication
edit- Drugs (such as opioids) that activate histamine (H1) receptors or trigger histamine release
- Chloroquine, a drug used in the treatment and prevention of malaria
- Bile acid congeners such as obeticholic acid
Related to pregnancy
edit- Gestational pemphigoid, a dermatosis of pregnancy
- Intrahepatic cholestasis of pregnancy, a medical condition in which cholestasis occurs
- Pruritic urticarial papules and plaques of pregnancy (PUPPP), a chronic hives-like rash
Other
edit- Menopause, or changes in hormonal balances associated with aging
- Terminal illness[18]
Mechanism
editItch can originate in the peripheral nervous system (dermal or neuropathic) or in the central nervous system (neuropathic, neurogenic, or psychogenic).[19][20][21]
Pruritoceptive
editItch originating in the skin is known as pruritoceptive, and can be induced by a variety of stimuli, including mechanical, chemical, thermal, and electrical stimulation, or infection. The primary afferent neurons responsible for histamine-induced itch are unmyelinated C-fibres.[1]
Nociceptors. Two major classes of human C-fibre nociceptors exist: mechano-responsive nociceptors and mechano-insensitive nociceptors. Mechano-responsive nociceptors have been shown in studies to respond to mostly pain, and mechano-insensitive receptors respond mostly to itch induced by histamine. However, it does not explain mechanically induced itch or itch produced without a flare reaction that involves no histamine.[1] Therefore, it is possible that pruritoceptive nerve fibres have different classes of fibres, which is unclear in current research.[2]
Histology and skin layers. Studies have been done to show that itch receptors are found only on the top two skin layers, the epidermis and the epidermal/dermal transition layers.[citation needed] Shelley and Arthur verified the depth by injecting individual itch powder (Mucuna pruriens) spicules and noting that maximal sensitivity occurred at the basal cell layer or the innermost layer of the epidermis. Surgical removal of those skin layers removed the ability for a patient to perceive itch.[citation needed] Itch is never felt in muscle or joints, which strongly suggests that deep tissue probably does not contain itch signaling apparatuses.[citation needed]
Sensitivity to pruritic stimuli is evenly distributed across the skin and has a clear spot distribution with similar density to that of pain. The different substances that elicit itch upon intracutaneous injection (injection within the skin) elicit only pain when injected subcutaneously (beneath the skin).[citation needed]
Molecular basis
editItch is often classified as that which is histamine mediated (histaminergic) and nonhistaminergic.
Itch is readily abolished in skin areas treated with nociceptor excitotoxin capsaicin but remains unchanged in skin areas rendered touch insensitive by pretreatment with anti-inflammatory saponins. Although experimentally induced itch can still be perceived under a complete A-fiber conduction block, it is significantly diminished. Overall, itch sensation is mediated by A-delta and C nociceptors located in the uppermost layer of the skin.[22]
Gene expression. Using single-cell mRNA sequencing, clusters of genes expressed in itch-related tissues were identified, e.g. NP1-3, transmitting itch information; where NP3 expresses neuropeptides Nppb and Sst as well as genes involved in inflammatory itch (Il31ra, Osmr and Crystrl2). The histamine receptor gene Hrh1 was found in NP2 and NP3, suggesting that histaminergic itch is transmitted by both these pruriceptive sub clusters.[23]
Infection. Staphylococcus aureus, a bacterial pathogen associated with itchy skin diseases, directly activates pruriceptor sensory neurons to drive itch. Skin exposure to S. aureus causes robust itch and scratch-induced damage. This reaction is mediated by S. aureus serine protease V8 which cleaves proteinase-activated receptor 1 (PAR1) on mouse and human sensory neurons. Targeting PAR1 through genetic deficiency, small interfering RNA (siRNA) knockdown, or pharmacological blockade decreases itch and skin damage caused by V8 and S. aureus exposure.[24]
Spinal itch pathway
editAfter the pruriceptive primary afferent has been activated, the signal is transmitted from the skin into the spinal dorsal horn. In this area, a number of interneurons will either be inhibited or activated to promote activation of projection neurons, mediating the pruriceptive signal to the brain. The GRP-GRPR interneuron system has been found to be important for mediating both histaminergic and non-histaminergic itch, where the GRP neurons activate GRPR neurons to promote itch [25][26]
Neuropathic
editNeuropathic itch can originate at any point along the afferent pathway as a result of damage of the nervous system. They could include diseases or disorders in the central nervous system or peripheral nervous system.[20] Examples of neuropathic itch in origin are notalgia paresthetica, brachioradial pruritus, brain tumors, multiple sclerosis, peripheral neuropathy, and nerve irritation.[27]
Neurogenic
editNeurogenic itch, which is itch induced centrally but with no neural damage, is mostly associated with increased accumulation of exogenous opioids and possibly synthetic opioids.[20]
Psychogenic
editItch is also associated with some symptoms of psychiatric disorders such as tactile hallucinations, delusions of parasitosis, or obsessive-compulsive disorders (as in OCD-related neurotic scratching).[20]
Peripheral sensitization
editInflammatory mediators—such as bradykinin, serotonin (5-HT) and prostaglandins—released during a painful or pruritic inflammatory condition not only activate pruriceptors but also cause acute sensitization of the nociceptors. In addition, expression of neuro growth factors (NGF) can cause structural changes in nociceptors, such as sprouting. NGF is high in injured or inflamed tissue. Increased NGF is also found in atopic dermatitis, a hereditary and non-contagious skin disease with chronic inflammation.[28] NGF is known to up-regulate neuropeptides, especially substance P. Substance P has been found to have an important role in inducing pain; however, there is no confirmation that substance P directly causes acute sensitization. Instead, substance P may contribute to itch by increasing neuronal sensitization and may affect release of mast cells, which contain many granules rich in histamine, during long-term interaction.[2]
Central sensitization
editNoxious input to the spinal cord is known to produce central sensitization, which consists of allodynia, exaggeration of pain, and punctuate hyperalgesia, extreme sensitivity to pain. Two types of mechanical hyperalgesia can occur: 1) touch that is normally painless in the uninjured surroundings of a cut or tear can trigger painful sensations (touch-evoked hyperalgesia), and 2) a slightly painful pin prick stimulation is perceived as more painful around a focused area of inflammation (punctuate hyperalgesia). Touch-evoked hyperalgesia requires continuous firing of primary afferent nociceptors, and punctuate hyperalgesia does not require continuous firing which means it can persist for hours after a trauma and can be stronger than normally experienced. In addition, it was found that patients with neuropathic pain, histamine ionophoresis resulted in a sensation of burning pain rather than itch, which would be induced in normal healthy patients. This shows that there is spinal hypersensitivity to C-fiber input in chronic pain.[2]
Treatment
editA variety of over-the-counter and prescription anti-itch drugs are available. Some plant products have been found to be effective anti-pruritics, others not. Non-chemical remedies include cooling, warming, soft stimulation.
Topical antipruritics in the form of creams and sprays are often available over-the-counter. Oral anti-itch drugs also exist and are usually prescription drugs. The active ingredients usually belong to the following classes:
- Antihistamines, such as diphenhydramine (Benadryl)[29]
- Corticosteroids, such as hydrocortisone topical cream; see topical steroid
- Counterirritants, such as mint oil, menthol, or camphor[30]
- Crotamiton (trade name Eurax) is an antipruritic agent available as a cream or lotion, often used to treat scabies. Its mechanism of action remains unknown.
- JAK inhibitors, such as ruxolitinib topical cream; see topical JAK inhibitor
- Local anesthetics, such as benzocaine topical cream (Lanacane)
Phototherapy is helpful for severe itching, especially if caused by chronic kidney disease. The common type of light used is UVB.[31]
Sometimes scratching relieves isolated itches, hence the existence of devices such as the back scratcher. Often, however, scratching only offers temporary relief and can intensify itching, even causing further damage to the skin, dubbed the "itch-scratch cycle".[32]
The mainstay of therapy for dry skin is maintaining adequate skin moisture and topical emollients.
No studies have been conducted to investigate the effectiveness of emollient creams, cooling lotions, topical corticosteroids, topical antidepressants, systemic antihistamines, systemic antidepressants, systemic anticonvulsants, and phototherapy on chronic pruritus of unknown origin.[29] However, there are clinical trials currently underway with dupilumab which is thought to alleviate itch by acting on the IL-4 receptor on sensory neurons.[33][34] The effectiveness of therapeutic options for people who are terminally ill with malignant cancer is not known.[18]
Epidemiology
editApproximately 280 million people globally, 4% of the population, have difficulty with itchiness.[35] This is comparable to the 2–3% of the population who have psoriasis.
History
editIn 1660, German physician Samuel Hafenreffer introduced the definition of pruritus (itch).[36]
See also
edit- Feeling, a perceptual state of conscious experience.
- Formication, a sensation that resembles that of small insects crawling on or under the skin
- Pruritus ani (also known as anusitis), irritation of skin at the exit of the rectum (anus), causing the desire to scratch
- Referred itch, a phenomenon in which a stimulus applied in one region of the body is felt as an itch or irritation in a different part of the body
- Itching powder, a powder or powder-like substance that induces itching when applied onto human skin.
References
edit- ^ a b c Andersen HH, Elberling J, Arendt-Nielsen L (September 2015). "Human surrogate models of histaminergic and non-histaminergic itch". Acta Dermato-Venereologica. 95 (7): 771–777. doi:10.2340/00015555-2146. PMID 26015312.
- ^ a b c d e f g Ikoma A, Steinhoff M, Ständer S, et al. (July 2006). "The neurobiology of itch". Nature Reviews. Neuroscience. 7 (7): 535–547. doi:10.1038/nrn1950. PMID 16791143. S2CID 9373105.
- ^ Greaves MW, Khalifa N (October 2004). "Itch: more than skin deep". International Archives of Allergy and Immunology. 135 (2): 166–172. doi:10.1159/000080898. PMID 15375326. S2CID 13376216.
- ^ a b Molkara S, Sabourirad S, Molooghi K (July 2019). "Infectious differential diagnosis of chronic generalized pruritus without primary cutaneous lesions: a review of the literature". International Journal of Dermatology. 59 (1): 30–36. doi:10.1111/ijd.14587. PMID 31364165. S2CID 198998956.
- ^ Harrison IP, Spada F (July 2019). "Breaking the Itch-Scratch Cycle: Topical Options for the Management of Chronic Cutaneous Itch in Atopic Dermatitis". Medicines. 6 (3): 76. doi:10.3390/medicines6030076. PMC 6789602. PMID 31323753.
- ^ Erickson S, Nahmias Z, Rosman IS, Kim BS (July 2018). "Immunomodulating Agents as Antipruritics". Dermatologic Clinics. 36 (3): 325–334. doi:10.1016/j.det.2018.02.014. PMID 29929604. S2CID 49336771.
- ^ Hinkle JL, Cheever KH (2018-08-30). Brunner and Suddarth's Textbook of Medical-Surgical Nursing. Wolters kluwer india Pvt Ltd. p. 1269. ISBN 978-93-87963-72-6. Archived from the original on 2023-09-23. Retrieved 2022-07-02.
- ^ Karsak M, Gaffal E, Date R, et al. (June 2007). "Attenuation of allergic contact dermatitis through the endocannabinoid system". Science. 316 (5830): 1494–1497. Bibcode:2007Sci...316.1494K. doi:10.1126/science.1142265. PMID 17556587. S2CID 37611370.
- ^ [citation needed]
- ^ Yosipovitch G, Fast K, Bernhard JD (December 2005). "Noxious heat and scratching decrease histamine-induced itch and skin blood flow". The Journal of Investigative Dermatology. 125 (6): 1268–1272. doi:10.1111/j.0022-202X.2005.23942.x. PMID 16354198.
- ^ Ward L, Wright E, McMahon SB (January 1996). "A comparison of the effects of noxious and innocuous counterstimuli on experimentally induced itch and pain". Pain. 64 (1): 129–138. doi:10.1016/0304-3959(95)00080-1. PMID 8867255. S2CID 25772165.
- ^ Pfützner W, Thomas P, Niedermeier A, et al. (2003-02-20). "Systemic contact dermatitis elicited by oral intake of Balsam of Peru". Acta Dermato-Venereologica. 83 (4): 294–295. doi:10.1080/00015550310016599. PMID 12926805.
- ^ Usatine RP, Riojas M (August 2010). "Diagnosis and management of contact dermatitis". American Family Physician. 82 (3). Aafp.org: 249–255. PMID 20672788. Archived from the original on 2014-04-09. Retrieved 2014-04-09.
- ^ Byers JP (2006). Metalworking Fluids (Second ed.). CRC Press. ISBN 142001773X. Archived from the original on 2023-01-12. Retrieved 2016-03-05.
- ^ Feingold BF (1973). Byers JP (ed.). Introduction to clinical allergy. the University of Michigan. ISBN 0398027978. Archived from the original on 2023-01-12. Retrieved 2020-06-24.
- ^ LaBagnara, James. eMedicine –Hyperparathyroidism Archived 2008-12-02 at the Wayback Machine. emedicine.com
- ^ Jovičić, Sanja; Balaban, Jagoda; Gajanin, Vesna (2023-06-24). "Association of systemic diseases with chronic pruritus". Scripta Medica. 54 (2): 163–167. doi:10.5937/scriptamed54-43882. ISSN 2490-3329.
- ^ a b Boehlke, Christopher; Joos, Lisa; Coune, Bettina; Becker, Carola; Meerpohl, Joerg J.; Buroh, Sabine; Hercz, Daniel; Schwarzer, Guido; Becker, Gerhild (2023-04-14). "Pharmacological interventions for pruritus in adult palliative care patients". The Cochrane Database of Systematic Reviews. 4 (2023): CD008320. doi:10.1002/14651858.CD008320.pub4. ISSN 1469-493X. PMC 11339634. PMID 37314034. Archived from the original on 2023-07-27. Retrieved 2023-07-27.
- ^ Yosipovitch G, Greaves MW, Schmelz M (February 2003). "Itch". Lancet. 361 (9358): 690–694. doi:10.1016/S0140-6736(03)12570-6. PMID 12606187. S2CID 208793207.
- ^ a b c d Twycross R, Greaves MW, Handwerker H, et al. (January 2003). "Itch: scratching more than the surface". QJM. 96 (1): 7–26. doi:10.1093/qjmed/hcg002. PMID 12509645.
- ^ "Essential pruritus". Archived from the original on 6 August 2020. Retrieved 25 July 2019.
- ^ Schmelz M, Schmidt R, Bickel A, et al. (October 1997). "Specific C-receptors for itch in human skin". The Journal of Neuroscience. 17 (20): 8003–8008. doi:10.1523/JNEUROSCI.17-20-08003.1997. PMC 6793906. PMID 9315918.
- ^ Usoskin D, Furlan A, Islam S, et al. (January 2015). "Unbiased classification of sensory neuron types by large-scale single-cell RNA sequencing". Nature Neuroscience. 18 (1): 145–153. doi:10.1038/nn.3881. PMID 25420068. S2CID 205437148.
- ^ Deng, Liwen; Costa, Flavia; Blake, Kimbria J.; Choi, Samantha; Chandrabalan, Arundhasa; Yousuf, Muhammad Saad; Shiers, Stephanie; Dubreuil, Daniel; Vega-Mendoza, Daniela; Rolland, Corinne; Deraison, Celine; Voisin, Tiphaine; Bagood, Michelle D.; Wesemann, Lucia; Frey, Abigail M.; Palumbo, Joseph S.; Wainger, Brian J.; Gallo, Richard L.; Leyva-Castillo, Juan-Manuel; Vergnolle, Nathalie; Price, Theodore J.; Ramachandran, Rithwik; Horswill, Alexander R.; Chiu, Isaac M. (2023). "S. aureus drives itch and scratch-induced skin damage through a V8 protease-PAR1 axis". Cell. 186 (24): 5375–5393.e25. doi:10.1016/j.cell.2023.10.019. PMC 10669764. PMID 37995657.
- ^ Han L, Ma C, Liu Q, et al. (February 2013). "A subpopulation of nociceptors specifically linked to itch". Nature Neuroscience. 16 (2): 174–182. doi:10.1038/nn.3289. PMC 3557753. PMID 23263443.
- ^ Sun YG, Chen ZF (August 2007). "A gastrin-releasing peptide receptor mediates the itch sensation in the spinal cord". Nature. 448 (7154): 700–703. Bibcode:2007Natur.448..700S. doi:10.1038/nature06029. PMID 17653196. S2CID 4407979.
- ^ Bernhard JD (2005). "Itch and pruritus: what are they, and how should itches be classified?". Dermatologic Therapy. 18 (4): 288–291. doi:10.1111/j.1529-8019.2005.00040.x. PMID 16296999. S2CID 7107271.
- ^ Rukwied R, Lischetzki G, McGlone F, et al. (June 2000). "Mast cell mediators other than histamine induce pruritus in atopic dermatitis patients: a dermal microdialysis study". The British Journal of Dermatology. 142 (6): 1114–1120. doi:10.1046/j.1365-2133.2000.03535.x. PMID 10848733. S2CID 23996950.
- ^ a b Andrade A, Kuah CY, Martin-Lopez JE, et al. (Cochrane Skin Group) (January 2020). "Interventions for chronic pruritus of unknown origin". The Cochrane Database of Systematic Reviews. 1 (1): CD013128. doi:10.1002/14651858.CD013128.pub2. PMC 6984650. PMID 31981369.
- ^ Hercogová J (2005). "Topical anti-itch therapy". Dermatologic Therapy. 18 (4): 341–343. doi:10.1111/j.1529-8019.2005.00033.x. PMID 16297007. S2CID 31573591.
- ^ El Mulla KF, Khalifa DE, Gawish RI, Eldeeb ME (2023). "Phototherapy versus pregabalin in treatment of chronic kidney disease associated pruritus: randomized controlled study". Journal of the Egyptian Women's Dermatologic Society. 20 (2): 81. doi:10.4103/jewd.jewd_50_22. ISSN 1687-1537.
- ^ Rinaldi G (April 2019). "The Itch-Scratch Cycle: A Review of the Mechanisms". Dermatology Practical & Conceptual. 9 (2): 90–97. doi:10.5826/dpc.0902a03. PMC 6502296. PMID 31106010.
- ^ Oetjen LK, Mack MR, Feng J, et al. (2017). "Sensory Neurons Co-opt Classical Immune Signaling Pathways to Mediate Chronic Itch". Cell. 171 (1): 217–228.e13. doi:10.1016/j.cell.2017.08.006. PMC 5658016. PMID 28890086.
- ^ "Efficacy and Safety of Subcutaneous Dupilumab for the Treatment of Adult Participants With Chronic Pruritus of Unknown Origin (CPUO) (LIBERTY-CPUO-CHIC)". ClinicalTrials.gov. NCT05263206. Archived from the original on 2023-01-14. Retrieved 2023-01-14.
- ^ Vos T, Flaxman AD, Naghavi M, et al. (Global Burden of Disease Study Collaborators) (December 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2163–2196. doi:10.1016/S0140-6736(12)61729-2. PMC 6350784. PMID 23245607.
- ^ Jean Bolognia; Joseph L. Jorizzo; Ronald P. Rapini (2008). Dermatology (2nd ed.). St. Louis, Mo.: Mosby/Elsevier. ISBN 978-1-4160-2999-1. OCLC 212399895.
Further reading
edit- Han L, Dong X (6 May 2014). "Itch mechanisms and circuits". Annual Review of Biophysics. 43 (1): 331–355. doi:10.1146/annurev-biophys-051013-022826. PMC 4081479. PMID 24819620.
- Andrew D, Craig AD (January 2001). "Spinothalamic lamina I neurons selectively sensitive to histamine: a central neural pathway for itch". Nature Neuroscience. 4 (1): 72–77. doi:10.1038/82924. PMID 11135647. S2CID 28727869.
- "Pruritus". National Cancer Institute. 2003. Archived from the original on 25 December 2005. Retrieved 22 August 2005.