A pulmonary artery is an artery in the pulmonary circulation that carries deoxygenated blood from the right side of the heart to the lungs. The largest pulmonary artery is the main pulmonary artery or pulmonary trunk from the heart, and the smallest ones are the arterioles, which lead to the capillaries that surround the pulmonary alveoli.
| Pulmonary artery | |
|---|---|
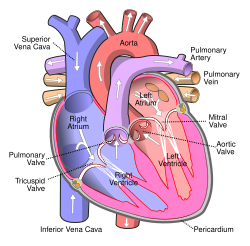 Anterior (frontal) view of the opened heart. White arrows indicate normal blood flow. (Pulmonary artery labelled at upper right.) | |
| Details | |
| Precursor | Truncus arteriosus |
| System | Cardiovascular, respiratory |
| Source | Right ventricle |
| Identifiers | |
| Latin | arteria pulmonalis |
| MeSH | D011651 |
| TA2 | 4074 |
| FMA | 66326 |
| Anatomical terminology | |
Structure
editThe pulmonary arteries are blood vessels that carry systemic venous blood from the right ventricle of the heart to the microcirculation of the lungs. Unlike in other organs where arteries supply oxygenated blood, the blood carried by the pulmonary arteries is deoxygenated, as it is venous blood returning to the heart. The main pulmonary arteries emerge from the right side of the heart and then split into smaller arteries that progressively divide and become arterioles, eventually narrowing into the capillary microcirculation of the lungs where gas exchange occurs.[citation needed]
Pulmonary trunk
editIn order of blood flow, the pulmonary arteries start as the pulmonary trunk that leaves the fibrous pericardium (parietal pericardium) of the ventricular outflow tract of right ventricle (also known as infundibulum or conus arteriosus.[1] The outflow track runs superiorly and to the left, posterior to the pulmonary valve.[1] The pulmonary trunk bifurcates into right and left pulmonary arteries below the arch of aorta and in front of the left main bronchus.[1] Pulmonary trunk is short and wide – approximately 5 centimetres (2.0 in) in length[2] and 2 centimetres (0.79 in)-3 centimetres (1.2 in) in diameter.[3][4]
The pulmonary trunk splits into the right and the left main pulmonary artery.[5] The left main pulmonary artery is shorter than the right,[1] passes behind and downwards the descending aorta and above the left main bronchus to the root of the left lung. Above, the left main pulmonary artery is connected to the concavity of the proximal descending aorta by the ligamentum arteriosum.[2] The right pulmonary artery pass across the midline of the body, below the carina of trachea, and comes in front of the right main bronchus.[1]
Branches
editThe left main pulmonary artery then divides into two lobar arteries, one for each lobe of the left lung.[6]
At the right root of the lung, it bifurcates into artery that supplies the right upper lobe of the lung, in front of the right upper lobe bronchus, and interlobar artery that supplies the right middle and inferior lobes of the lung, running together with bronchus intermedius.[1]
The right and left main pulmonary (lungs) arteries give off branches that supplies the corresponding lung lobes. In such cases it is termed lobar arteries.[7] The lobar arteries branch into segmental arteries (roughly 1 for each segment). Segmental arteries run together with segmental bronchi, at the posterolateral surfaces of the bronchi.[7] These in turn branch into subsegmental pulmonary arteries.[7] These eventually form intralobular arteries.[8] The pulmonary arteries supply the alveoli of the lungs. In contrast, bronchial arteries, that has different origins, supply the bronchi of the lungs.[1]
Development
editThe pulmonary arteries originate from the truncus arteriosus and the sixth pharyngeal arch. The truncus arteriosus is a structure that forms during the development of the heart as a successor to the conus arteriosus.[9]: 157
By the third week of development, the endocardial tubes have developed a swelling in the part closest to the heart. The swelling is known as the bulbus cordis and the upper part of this swelling develops into the truncus arteriosus.[9]: 159–160 The structure is ultimately mesodermal in origin.[9]: 157 During development of the heart, the heart tissues undergo folding, and the truncus arteriosus is exposed to what will eventually be both the left and right ventricles. As a septum develops between the two ventricles of the heart, two bulges form on either side of the truncus arteriosus. These progressively enlarge until the trunk splits into the aorta and pulmonary arteries.[9]: 176–179 Failure of these processes can lead to pulmonary artery agenesis.
During early development, the ductus arteriosus connects the pulmonary trunk and the aortic arch, allowing blood to bypass the lungs.[10]: 791
Function
editThe pulmonary artery carries deoxygenated blood from the right ventricle to the lungs.[11] The blood here passes through capillaries adjacent to alveoli and becomes oxygenated as part of the process of respiration.[12]
In contrast to the pulmonary arteries, the bronchial arteries supply nutrition to the lungs themselves.[10]: 790
Pressure
editThe pulmonary artery pressure (PA pressure) is a measure of the blood pressure found in the main pulmonary artery. This is measured by inserting a catheter into the main pulmonary artery.[13] : 190–191 The mean pressure is typically 9–18 mmHg,[14] and the wedge pressure measured in the left atrium may be 6–12 mmHg. The wedge pressure may be elevated in left heart failure,[13]: 190–191 mitral valve stenosis, and other conditions, such as sickle cell disease.[15]
Clinical significance
editThe pulmonary artery is relevant in a number of clinical states. Pulmonary hypertension is used to describe an increase in the pressure of the pulmonary artery, and may be defined as a mean pulmonary artery pressure of greater than 25 mmHg.[13]: 720 A pulmonary artery diameter of more than 29 mm (measured on a CT scan) is often used as an indicator for pulmonary hypertension.[16] In chest X-rays, a diameter of more than 16 mm for the right descending pulmonary artery is also an indicator for pulmonary hypertension.[17] This may occur as a result of heart problems such as heart failure, lung or airway disease such as COPD or scleroderma, or thromboembolic disease such as pulmonary embolism or emboli seen in sickle cell anaemia.[13]: 720–721 Most recently, computational fluid based tools (non-invasive) have been proposed to be at par with the current clinical tests (invasive) of pulmonary hypertension.[18]
Pulmonary embolism refers to an embolus that lodges in the pulmonary circulation. This may arise from a deep venous thrombosis, especially after a period of immobility. A pulmonary embolus is a common cause of death in patients with cancer and stroke.[13]: 720–721 A large pulmonary embolus that becomes lodged in the bifurcation of the pulmonary trunk with extensions into both the left and right main pulmonary arteries is called a saddle embolus.[19]
Several animal models have been utilized for investigating pulmonary artery related pathologies. Porcine model of pulmonary artery is the most frequently used and it was recently found that their mechanical properties vary with every subsequent branching.[20]
Additional images
edit-
Image showing main pulmonary artery coursing ventrally to the aortic root and trachea, and the right pulmonary artery passes dorsally to the ascending aorta, while the left pulmonary artery passes ventrally to the descending aorta.
-
Pulmonary circuit
-
Transverse section of thorax, showing relations of pulmonary artery.
-
Pulmonary artery
-
Pulmonary artery.Deep dissection.Anterior view.
-
CT scan of a normal lung, with different levels of pulmonary arteries.
-
Bronchial anatomy
See also
editReferences
edit- ^ a b c d e f g Ryan, Stephanie (2011). "2". Anatomy for diagnostic imaging (Third ed.). Elsevier Ltd. pp. 126, 133. ISBN 9780702029714.
- ^ a b Cheitlin MD, Ursell PC (2011). "Cardiac Anatomy". In Chatterjee K (ed.). Cardiology: An Illustrated Textbook. JP Medical Ltd. p. 6. ISBN 9789350252758.
- ^ Edwards, P D; Bull, R K; Coulden, R (1998-10-01). "CT measurement of main pulmonary artery diameter". The British Journal of Radiology. 71 (850): 1018–1020. doi:10.1259/bjr.71.850.10211060. ISSN 0007-1285. PMID 10211060.
- ^ Truong, Quynh A.; Massaro, Joseph M.; Rogers, Ian S.; Mahabadi, Amir A.; Kriegel, Matthias F.; Fox, Caroline S.; O'Donnell, Christopher J.; Hoffmann, Udo (2012-01-01). "Reference Values for Normal Pulmonary Artery Dimensions by Noncontrast Cardiac Computed Tomography". Circulation: Cardiovascular Imaging. 5 (1): 147–154. doi:10.1161/CIRCIMAGING.111.968610. PMC 3275437. PMID 22178898.
- ^ "Pulmonary Vasculature". University of Virginia School of Medicine. 2013. Retrieved 2017-06-24.
- ^ Kandathil, Asha; Chamarthy, Murthy (June 2018). "Pulmonary vascular anatomy & anatomical variants". Cardiovascular Diagnosis and Therapy. 8 (3): 201–207. doi:10.21037/cdt.2018.01.04. ISSN 2223-3652. PMC 6039811. PMID 30057869.
- ^ a b c "Pulmonary Artery Anatomy". University of Virginia School of Medicine. 2013. Retrieved 2017-06-24.
- ^ Takahashi M, Fukuoka J, Nitta N, Takazakura R, Nagatani Y, Murakami Y, et al. (2008). "Imaging of pulmonary emphysema: a pictorial review". International Journal of Chronic Obstructive Pulmonary Disease. 3 (2): 193–204. doi:10.2147/COPD.S2639. PMC 2629965. PMID 18686729.
- ^ a b c d Schoenwolf GC, Larsen MJ, Bleyl SR, Brauer PR, Francis-West PH (2009). Larsen's human embryology (4th ed., Thoroughly rev. and updated. ed.). Philadelphia: Churchill Livingstone/Elsevier. pp. Development of the Urogenital system. ISBN 9780443068119.
- ^ a b Braunwald E (1992). Heart Disease: A Textbook of Cardiovascular Medicine (Fourth ed.). Philadelphia: W.B. Sanders.
- ^ "22.4 Gas Exchange – Anatomy and Physiology". opentextbc.ca. Archived from the original on 2020-10-19. Retrieved 2019-05-22.
- ^ "Exchanging Oxygen and Carbon Dioxide – Lung and Airway Disorders". MSD Manual Consumer Version. Retrieved 2019-05-22.
- ^ a b c d e Colledge NR, Walker BR, Ralston SH, Britton R, eds. (2010). Davidson's Principles and Practice of Medicine (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. ISBN 978-0-7020-3084-0.
- ^ "Normal Hemodynamic Parameters – Adult" (PDF). Edwards Lifesciences LLC. Archived from the original (PDF) on 2010-11-10.
- ^ Pashankar FD, Carbonella J, Bazzy-Asaad A, Friedman A (April 2008). "Prevalence and risk factors of elevated pulmonary artery pressures in children with sickle cell disease". Pediatrics. 121 (4): 777–782. doi:10.1542/peds.2007-0730. PMID 18381543. S2CID 26693444.
- ^ Marini TJ, He K, Hobbs SK, Kaproth-Joslin K (December 2018). "Pictorial review of the pulmonary vasculature: from arteries to veins". Insights into Imaging. 9 (6): 971–987. doi:10.1007/s13244-018-0659-5. PMC 6269336. PMID 30382495.
- ^ Chang CH (December 1965). "The normal roentgenographic measurement of the right descending pulmonary artery in 1,085 cases and its clinical application. II. Clinical application of the measurement of the right descending pulmonary artery in the radiological diagnosis of pulmonary hypertensions from various causes" (PDF). Nagoya Journal of Medical Science. 28 (1): 67–80. PMID 5865788. Retrieved 15 January 2022.
- ^ Piskin S, Patnaik SS, Han D, Bordones AD, Murali S, Finol EA (March 2020). "A canonical correlation analysis of the relationship between clinical attributes and patient-specific hemodynamic indices in adult pulmonary hypertension". Medical Engineering & Physics. 77: 1–9. doi:10.1016/j.medengphy.2020.01.006. PMC 7069525. PMID 32007361.
- ^ Jones J, et al. "Saddle pulmonary embolism". Radiopaedia. Retrieved 2017-10-08.
- ^ Pillalamarri NR, Patnaik SS, Piskin S, Gueldner P, Finol EA (January 2021). "Ex Vivo Regional Mechanical Characterization of Porcine Pulmonary Arteries". Experimental Mechanics. 61 (1): 285–303. doi:10.1007/s11340-020-00678-2. PMC 8011683. PMID 33814554.
External links
edit- Anatomy photo:20:01-0106 at the SUNY Downstate Medical Center – "Heart: The Pericardial sac and Great vessels"
- Anatomy photo:20:07-0105 at the SUNY Downstate Medical Center – "Heart: Openings of Great Vessels into the Pericardial Sac"
- Anatomy figure: 19:05-06 at Human Anatomy Online, SUNY Downstate Medical Center – "Mediastinal surface of the right lung"
- Anatomy figure: 19:06-02 at Human Anatomy Online, SUNY Downstate Medical Center – "Mediastinal surface of the left lung"
- Histology image: 13802loa – Histology Learning System at Boston University