Pancreatic serous cystadenoma is a benign tumour of the pancreas.[2] It is usually solitary and found in the body or tail of the pancreas, and may be associated with von Hippel–Lindau syndrome.[2]
| Pancreatic serous cystadenoma | |
|---|---|
| Other names | Serous cystadenoma of the pancreas, serous microcystic adenoma |
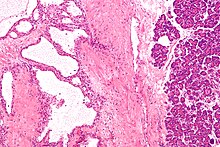 | |
| Micrograph showing a pancreatic serous cystadenoma. H&E stain. | |
| Specialty | General surgery, gastroenterology |
| Symptoms | Usually asymptomatic |
| Usual onset | 50–60 years of age |
| Risk factors | Female gender |
| Treatment | Surgical resection (if symptomatic) |
| Deaths | 0.1%[1] |
In contrast to some of the other cyst-forming tumors of the pancreas (such as the intraductal papillary mucinous neoplasm and the pancreatic mucinous cystadenoma), serous cystic neoplasms are almost always entirely benign. There are some exceptions; rare case reports have described isolated malignant serous cystadenocarcinomas.[3] In addition, serous cystic neoplasms slowly grow, and if they grow large enough they can press on adjacent organs and cause symptoms.
Signs and symptoms
editIn most cases, serous cystadenomas of the pancreas are asymptomatic.[4] However, large cysts may cause symptoms related to their size.[4]
Classification
editPathologists classify serous cystic neoplasms into two broad groups. Those that are benign, that have not spread to other organs, are designated "serous cystadenoma".[5] Serous cystadenomas can be further sub-typed into microcystic, oligocystic (or macrocystic), solid, mixed serous-endocrine neoplasm, and VHL-associated serous cystic neoplasm. This latter classification scheme is useful because it highlights the range of appearances and the clinical associations of these neoplasms. Serous cystic neoplasms that have spread ("metastasized") to another organ are considered malignant and are designated "serous cystadenocarcinoma".[citation needed]
Pathology
editTreatment
editThese lesions rarely require surgery unless they are symptomatic or the diagnosis is in question. Since these lesions do not have malignant potential, long-term observation with imaging surveillance is unnecessary.[4] Surgery can include the removal of the head of the pancreas (a pancreaticoduodenectomy), removal of the body and tail of the pancreas (a distal pancreatectomy), or rarely removal of the entire pancreas (a total pancreatectomy).[6] In selected cases the surgery can be performed using minimally invasive techniques such as laparoscopy.[7]
Epidemiology
editSerous cystadenomas of the pancreas are more common in women.[4] SCAs are usually diagnosed in people 50–60 years of age.[4]
See also
editReferences
edit- ^ Jais B, Rebours V, Malleo G, Salvia R, Fontana M, Maggino L, et al. (February 2016). "Serous cystic neoplasm of the pancreas: a multinational study of 2622 patients under the auspices of the International Association of Pancreatology and European Pancreatic Club (European Study Group on Cystic Tumors of the Pancreas)". Gut. 65 (2): 305–312. doi:10.1136/gutjnl-2015-309638. hdl:11577/3187425. PMID 26045140. S2CID 206962150.
- ^ a b WHO Classification of Tumours Editorial Board (2019). "10. Tumours of the pancreas: Pancreatic serous cystadenoma". Digestive System Tumours. Vol. 1 (5th ed.). Lyon (France). pp. 303–306. ISBN 978-92-832-4499-8.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Galanis C, Zamani A, Cameron JL, Campbell KA, Lillemoe KD, Caparrelli D, et al. (July 2007). "Resected serous cystic neoplasms of the pancreas: a review of 158 patients with recommendations for treatment". Journal of Gastrointestinal Surgery. 11 (7): 820–826. doi:10.1007/s11605-007-0157-4. PMID 17440789. S2CID 32023143.
- ^ a b c d e Elta GH, Enestvedt BK, Sauer BG, Lennon AM (April 2018). "ACG Clinical Guideline: Diagnosis and Management of Pancreatic Cysts". The American Journal of Gastroenterology. 113 (4): 464–479. doi:10.1038/ajg.2018.14. PMID 29485131. S2CID 3584079.
- ^ "Pathology of Neoplasms of the Pancreas". Johns Hopkins University. Retrieved 25 April 2010.
- ^ "Pancreatic Surgery". Johns Hopkins University. Retrieved 25 April 2010.
- ^ "Laproscopic Pancreatic Surgery". Johns Hopkins University. Retrieved 25 April 2010.
- ^ Wang Y, Miller FH, Chen ZE, Merrick L, Mortele KJ, Hoff FL; et al. (2011). "Diffusion-weighted MR imaging of solid and cystic lesions of the pancreas". Radiographics. 31 (3): E47-64. doi:10.1148/rg.313105174. PMID 21721197.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
Diagram by Mikael Häggström, M.D.