A ventilation/perfusion lung scan, also called a V/Q lung scan, or ventilation/perfusion scintigraphy, is a type of medical imaging using scintigraphy and medical isotopes to evaluate the circulation of air and blood within a patient's lungs,[1][2] in order to determine the ventilation/perfusion ratio. The ventilation part of the test looks at the ability of air to reach all parts of the lungs, while the perfusion part evaluates how well blood circulates within the lungs. As Q in physiology is the letter used to describe bloodflow the term V/Q scan emerged.
| Ventilation/perfusion scan | |
|---|---|
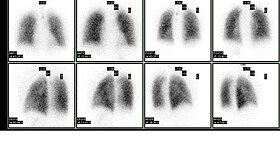 Normal pulmonary ventilation and perfusion (V/Q) scan. The nuclear medicine V/Q scan is useful in the evaluation of pulmonary embolism. | |
| OPS-301 code | 3-703.2 |
Uses
editThis test is most commonly done in order to check for the presence of a blood clot or abnormal blood flow inside the lungs (such as a pulmonary embolism (PE) although computed tomography with radiocontrast is now more commonly used for this purpose.[3][4] The V/Q scan may be used in some circumstances where radiocontrast would be inappropriate, as in allergy to contrast agent or kidney failure.[5]
A V/Q lung scan may be performed in the case of serious lung disorders such as chronic obstructive pulmonary disease (COPD) or pneumonia as well as a lung performance quantification tool pre- and post-lung lobectomy surgery.[6]
Significance of results
edit| Result | Interpretation | Significance |
|---|---|---|
| Normal | No perfusion deficit | Excludes pulmonary thromboembolism |
| Low probability | Perfusion deficit with matched ventilation deficit | < 20% probability of PE |
| Intermediate probability | Perfusion deficit that corresponds to parenchymal abnormality on chest x-ray | 20% - 80% probability of PE |
| High probability | Multiple segmental perfusion deficits with normal ventilation | > 80% probability of PE |
Decreased uptake of the inhaled radioisotope may indicate an impaired ability to breathe, airway obstruction, or possible pneumonia.
Decreased circulation of the injected MAA indicates a problem with blood flow into or within the lungs. A localized area of decreased uptake, usually in a wedge shaped (or pie shaped) configuration with normal ventilation images (mismatched defect) suggests a pulmonary embolus or blood clot in the lungs, which leads to reduced perfusion beyond the obstruction.
Risks
editAlthough this test uses radioactive materials, the total amount of radiation exposure is low. Typical effective doses for a V/Q scan range from 1-5 mSv.[7][8] In order to decrease the radiation exposure in pregnant patients, the total radioactivity administered may be decreased or the ventilation phase omitted. A CT pulmonary angiogram (CTPA) with radiocontrast can alternatively be performed, although this can result in a greater radiation dose to the patient.[9]
Procedure
editThe ventilation and perfusion phases of a V/Q lung scan are performed together and may include a chest X-ray for comparison or to look for other causes of lung disease. A defect in the perfusion images requires a mismatched ventilation defect to indicate pulmonary embolism.[8]
In the ventilation phase of the test, a gaseous radionuclides such as xenon-133, krypton-81m, or technetium-99m DTPA in an aerosol form is inhaled by the patient through a mouthpiece or mask that covers the nose and mouth.[10] Ventilation imaging can also be performed using a Technegas machine which produces an aerosol of radioactive nanoparticles, specifically carbon nanoparticles containing technetium-99m.[11] The perfusion phase of the test involves the intravenous injection of radioactive technetium macro aggregated albumin (Tc99m-MAA). A gamma camera acquires the images for both phases of the study.[12] A SPECT image can also be taken following an injection of Technetium labelled MAA. SPECT is often skipped if the patient has pulmonary hypertension.
It is also possible to perform the scan with positron emission tomography (PET) rather than conventional gamma camera scintigraphy.[13] This has been performed with Gallium-68 labelled carbon nanoparticles (Galligas) using a conventional Technegas machine for ventilation images, and with Gallium-68 labelled MAA (Ga68-MAA) for perfusion images. PET has multiple potential advantages including superior resolution, speed and quantification.[14][15]
See also
editReferences
edit- ^ "Pulmonary ventilation/perfusion scan". University of Maryland Medical Center. Retrieved 3 January 2018.
- ^ Mortensen, Jann; Berg, Ronan M.G. (1 January 2019). "Lung Scintigraphy in COPD" (PDF). Seminars in Nuclear Medicine. 49 (1): 16–21. doi:10.1053/j.semnuclmed.2018.10.010. PMID 30545511. S2CID 56486118. Retrieved 4 July 2021.
- ^ Konstantinides, Stavros V.; Torbicki, Adam; Agnelli, Giancarlo; Danchin, Nicolas; Fitzmaurice, David; Galiè, Nazzareno; Gibbs, J. Simon R.; Huisman, Menno V.; Humbert, Marc; Kucher, Nils; Lang, Irene; Lankeit, Mareike; Lekakis, John; Maack, Christoph; Mayer, Eckhard; Meneveau, Nicolas; Perrier, Arnaud; Pruszczyk, Piotr; Rasmussen, Lars H.; Schindler, Thomas H.; Svitil, Pavel; Vonk Noordegraaf, Anton; Zamorano, Jose Luis; Zompatori, Maurizio; Zamorano, Jose Luis; Achenbach, Stephan; Baumgartner, Helmut; Bax, Jeroen J.; Bueno, Hector; et al. (14 November 2014). "2014 ESC Guidelines on the diagnosis and management of acute pulmonary embolism" (PDF). European Heart Journal. 35 (43): 3033–3073. doi:10.1093/eurheartj/ehu283. PMID 25173341.
- ^ "Managing suspected pulmonary embolism". NICE. National Institute for Health and Care Excellence. January 2015.
- ^ Nigel Key; Michael Makris; Denise O'Shaughnessy; David Lillicrap (3 July 2009). Practical Hemostasis and Thrombosis. John Wiley and Sons. pp. 140–. ISBN 978-1-4051-8460-1. Retrieved 14 November 2010.
- ^ Mason, Robert J.; Broaddus, V. Courtney; Martin, Thomas R.; King, Talmadge E.; Schraufnagel, Dean; Murray, John F.; Nadel, Jay A. (2010). Murray and Nadel's Textbook of Respiratory Medicine. Elsevier Health Sciences. p. 477. ISBN 978-1437735536.
- ^ Parker, J. A.; Coleman, R. E.; Grady, E.; Royal, H. D.; Siegel, B. A.; Stabin, M. G.; Sostman, H. D.; Hilson, A. J. W. (26 January 2012). "SNM Practice Guideline for Lung Scintigraphy 4.0". Journal of Nuclear Medicine Technology. 40 (1): 57–65. doi:10.2967/jnmt.111.101386. PMID 22282651.
- ^ a b Bajc, M.; Neilly, J. B.; Miniati, M.; Schuemichen, C.; Meignan, M.; Jonson, B. (27 June 2009). "EANM guidelines for ventilation/perfusion scintigraphy". European Journal of Nuclear Medicine and Molecular Imaging. 36 (8): 1356–1370. doi:10.1007/s00259-009-1170-5. hdl:2158/774307. PMID 19562336.
- ^ Anderson, David R.; Kahn, Susan R.; Rodger, Marc A.; Kovacs, Michael J.; Morris, Tim; Hirsch, Andrew; Lang, Eddy; Stiell, Ian; Kovacs, George; Dreyer, Jon; Dennie, Carol; Cartier, Yannick; Barnes, David; Burton, Erica; Pleasance, Susan; Skedgel, Chris; O’Rouke, Keith; Wells, Philip S. (19 December 2007). "Computed Tomographic Pulmonary Angiography vs Ventilation-Perfusion Lung Scanning in Patients With Suspected Pulmonary Embolism". JAMA. 298 (23): 2743–53. doi:10.1001/jama.298.23.2743. PMID 18165667.
- ^ Fogelman, Ignac; Clarke, Susan; Cook, Gary; Gnanasegaran, Gopinath (2014). Atlas of Clinical Nuclear Medicine (3rd ed.). CRC Press. p. 1075. ISBN 9781841847528.
- ^ Lobov, Sergei A.; King, David W.; Knox, Karen J.; Senden, Tim J.; Stephens, Ross W. (February 2013). "Cationised radiolabelled nanoparticles for perfusion imaging of the lungs". Biomaterials. 34 (6): 1732–1738. doi:10.1016/j.biomaterials.2012.11.022. PMID 23218595.
- ^ Waxman, AD; Bajc, M; Brown, M; Fahey, FH; Freeman, LM; Haramati, LB; Julien, P; Le Gal, G; Neilly, B; Rabin, J; Soudry, G; Tapson, V; Torbati, S; Kauffman, J; Ahuja, S; Donohoe, K (May 2017). "Appropriate Use Criteria for Ventilation-Perfusion Imaging in Pulmonary Embolism: Summary and Excerpts" (PDF). Journal of Nuclear Medicine. 58 (5): 13N–15N. PMID 28461589.
- ^ Hofman, M. S.; Beauregard, J. -M.; Barber, T. W.; Neels, O. C.; Eu, P.; Hicks, R. J. (2011). "68Ga PET/CT Ventilation-Perfusion Imaging for Pulmonary Embolism: A Pilot Study with Comparison to Conventional Scintigraphy". Journal of Nuclear Medicine. 52 (10): 1513–1519. doi:10.2967/jnumed.111.093344. PMID 21908388.
- ^ Bailey, Dale L.; Eslick, Enid M.; Schembri, Geoffrey P.; Roach, Paul J. (September 2016). "68Ga PET Ventilation and Perfusion Lung Imaging—Current Status and Future Challenges". Seminars in Nuclear Medicine. 46 (5): 428–435. doi:10.1053/j.semnuclmed.2016.04.007. PMID 27553468.
- ^ Velikyan, Irina (2014). "Prospective of Ga-Radiopharmaceutical Development". Theranostics. 4 (1): 47–80. doi:10.7150/thno.7447. PMC 3881227. PMID 24396515.