This article needs attention from an expert in psychology. See the talk page for details. (January 2015) |
Zouhuorumo (Chinese: 走火入魔; pinyin: zǒuhuǒrùmó, meaning "obsession; spirit, possession, obsessing mind) refers to psychosomatic issues that can arise from excessive practice of self-cultivation techniques In Chinese culture, this concept traditionally signifies a disturbance or problem that occurs during spiritual or martial arts training. Within the qigong and traditional Chinese medical communities, zouhuorumo describes a physiological or psychological disorder believed to stem from the combination of a underlying predisposition and improper practice of these techniques. The term gained prominence in the 1980s and 1990s during the widespread popularity of qigong in China, called qigong fever. In Buddhist and Daoist circles, zouhuorumo is also used to describe individuals who engage in esoteric teachings, techniques, or meditations without possessing good character, established discipline, or proper guidance from a teacher.
Terminology
editThe Chinese term is zǒuhuǒrùmó (走火入魔, "be obsessed with [something]; possessed by the Devil"). In Traditional Chinese medicine, it is viewed as excessive heat moving upwards to the head, causing excessive emotion and thinking. The term is a compound of the words zouhuo (Chinese: 走火; pinyin: zǒuhuǒ, meaning a spark, to have a short circuit, overstate, overconsume, catch fire; to be on fire") and rumo (Chinese: 入魔; pinyin: rùmó, to be spellbound, to be infatuated/obsessed, fixated.[1]
In recent medical terminology, zouhuorumo includes what is known as "qigong deviation": qigongpiancha (simplified Chinese: 气功偏差; traditional Chinese: 氣功偏差; pinyin: qìgōngpiānchā).[2][3]
Background
editChinese medical practitioners, as well as Buddhist and Daoist nuns and monks, considered zouhuorumo a form of psychosis resulting from overly intense study of cultivation techniques by both clergy and laypeople. In the construct of Traditional Chinese medicine, this was thought to be caused by an imbalance or contravention of Shen ( 神, "mind; spirit") and or deficiency of Jing ( 精, "essence"), which are different classifications of qi.[4] In evidence based medicine, zouhuorumo refers to a number of undesirable somatic or psychological effects caused by qigong practices. In most cases the cause is unknown, short-lived and never receive medical attention.[5]
While self-cultivation techniques may act as a stressor in some vulnerable individuals, the relationships between this for of practice and various disorders are complex, and causal connections have not been demonstrated.[6] Similar syndromes have been observed in other forms of self-cultivation practices such as yoga (Kundalini syndrome),[7] meditation,[8] and hypnosis.[9]
Symptoms
editSymptoms are often identified as being in one of three categories:
- panic, anxiety, discomfort, and uncontrolled spontaneous movement, rigors and convulsions.
- sensory problems, such as visual or auditory hallucination
- irrational beliefs, psychosis and paranoia [10]
Somatic symptoms can include sensations and pain in head, chest and back, abdomen, limbs, or whole body; whereas, mental and emotional symptoms can include neurasthenia, affective disorder, self-consciousness, hallucination, and paranoia.[11]: 165–167
Diagnosis
editWhile the Chinese Society of Psychiatry prefers the term "qigong deviation", the American Psychiatric Association uses psychosis terminology.[12] Some physicians believe that this condition can be categorized as a culture-bound syndrome, but this point is debated.[13]
Chinese psychiatry
editIn the second edition of the Chinese Classification of Mental Disorders (CCMD-2) published by the Chinese Society of Psychiatry[14] the diagnosis of "Qigong Deviation Syndrome" is based upon the following criteria:[15]
- The subject being demonstrably normal before doing qigong exercises
- Psychological and physiological reactions appearing during or after qigong exercises (suggestion and autosuggestion may play an important role in these reactions)
- Complaints of abnormal sensations during or after qigong exercises
- Diagnostic criteria do not meet other mental disorders such as schizophrenia, affective disorder, and neurosis.
Western psychiatry
editIn the West, there was no equivalent experience until the adoption of qigong practices by the public became more common. When the Western medical community encountered abnormal conditions presenting in patients practicing qigong, they used the term "Qi-gong psychotic reaction" and classified the disorder as a culture-bound syndrome in the 4th edition of the Diagnostic and Statistical Manual (DSM-IV) of the American Psychiatric Association. It is described as
[a] term describing an acute, time-limited episode characterized by dissociative, paranoid, or other psychotic or non-psychotic symptoms that may occur after participation in the Chinese folk health-enhancing practice of qigong. Especially vulnerable are individuals who become overly involved in the practice.[16][17][18][19]
In order to diagnose this syndrome in the West, practitioners determine the cultural formation of the patient; this includes their cultural reference group and how that culture might explain their illness.[20]
The DSM-IV classification has been criticized by other Western psychiatrists on the grounds that
[i]t is not clear how the architects of the DSM-IV can logically defend labeling a syndrome as aberrant in the context of a diagnostic system while simultaneously placing that syndrome outside of conventional Western nosologic categories that serve as basis for determining whether a syndrome is or is not aberrant and therefore a disorder.[21]
Medical causes
editThe appearance of symptoms during or after qigong practice has been explained in various ways by the psychiatric community, in severe cases as an indication of latent psychosis. The Chinese medical literature includes a wider variety syndromes and their symptoms associated with qigong deviation; the non-psychotic symptoms correspond to conversion disorder and histrionic personality disorder in Western classifications.[22]
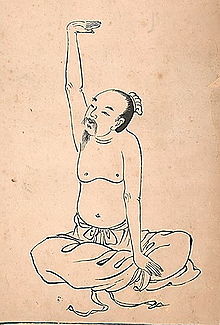
In traditional Chinese medicine this disorder is classified as a Shen (神) syndrome and has herbal and acupuncture treatments that date back thousand of years aimed at treating the spirit, mind and body that has been affected by excessive cultivation practices within meditation, Daoyin and Qigong.[23]
Traditionally in Chinese medicine the motivation for the practice of cultivation practice that being qigong, meditation or daoyin is a very important contributor to the development of Zouhuorumo . The wanting of a quick success for mastery for special powers, escapism, greed for money and fame, are all deviations from development of a noble human attitude and lifes endeavours.[24]
Latent psychosis
editIn cases of psychosis, Western and Eastern psychiatric belief is that qigong could be a precipitating stressor of a latent psychotic disorder to which the patient is predisposed, rather than erroneous qigong practice;[22] a type of reactive psychosis or the precipitation of an underlying mental illness, and is traditionally seen as a contraindication for self guided cultivation study and should be guided and consulted by a experienced practitioner or health professional. Some of the conditions are schizophrenia, bipolar disorder, or posttraumatic stress disorder.[25][26]
Qigong community perspective
editWithin the qigong community, Zou huo ru mo is believed to be caused by improper practice:[27]
- Inexperienced or unqualified instructor
- Incorrect instructions
- Impatience
- Becoming frightened, irritated, confused, or suspicious during the course of qigong practice
- Inappropriate focus, interpreted as "inappropriate channeling of qi (life energy)."
Treatment and prevention
editWithin the qigong community, there are specific traditional Chinese medical treatments believed to be effective for addressing different forms of Zou huo ru mo.
For the prevention of creating future problems those that have a tendency toward heat symptoms, hot head, sharp headaches, flushed face, easily excited, anxiety and over creative imaginations, should practise extensively lower, slower grounding movements, and conversely those that have more predominant cold symptoms including cold extremities, dull headaches, prone to melancholy and dull thinking should as a foundation of practice use standing, faster movements and techniques that lift the qi.[27]
In particular, depending upon somatic (body) versus psychological (mind) symptoms, and whether the condition is considered temporary or an intrinsic mental disorder, self-correction treatments can involve relaxation, walking, self-vibrating, self-patting, and self-massage. Clinical treatments can involve psychological counseling, expert guidance of practice, acupuncture, herbal, massage, "external qi" treatments, that are aimed at symptomatic and casual correction.[11]: 164–173
Social and political context
editSelf cultivation standing and seated meditation technology has a long history in East Asia and as a consequence has developed a specific specialised language based on observation of historical outcomes the term 走火入魔 is a general categorization for many adverse effects and classical syndromes of improper practice. Qigong deviation is a more modern term that became part of politically motivated agenda during the 1990s, when the Chinese government became concerned about loss of state control due to widespread popularity of qigong, mass practice, commercialization and rise to power of charismatic qigong "grandmasters" and fraudsters alike.[10][28][29]
References
edit- ^ DeFrancis, John (2003). ABC Chinese-English Comprehensive Dictionary. Honolulu: University of Hawaii Press. p. 1327, 1327, 783.
- ^ Mitchell, Damo (2018). A Comprehensive Guide to Daoist Nei Gong. Philadelphia: Jessica Kingsley Publishers. p. 517. ISBN 9780857013729. Retrieved 3 August 2023.
- ^ Chiang, Howard (2019). The Making of the Human Sciences in China: Historical and Conceptual Foundations. Boston: Brill. p. 498. ISBN 9789004397620. Retrieved 3 August 2023.
- ^ Lin, Zixin (2010). Qigong: Chinese Medicine Or Pseudoscience?. New York: Prometheus. p. 138. ISBN 9781616140717. Retrieved 3 August 2023.
- ^ Lee, Sing (December 1996). "Cultures in psychiatric nosology: the CCMD-2-R and international classification of mental disorders". Culture, Medicine and Psychiatry. 20 (4): 421–472. doi:10.1007/bf00117087. PMID 8989986. S2CID 25418717.
- ^ Ng BY. 1998. "Qigong-induced mental disorders: a review." Australian & New Zealand Journal of Psychiatry 33(2):197-206.
- ^ Upadhyaya, Pt.Rajnikant (2006). Awake Kundalini. Lotus Press. p. 26. ISBN 978-81-8382-039-4.
- ^ Nelson, James M. (2009). Psychology, Religion, and Spirituality. Springer. p. 470. ISBN 978-0-387-87572-9.
- ^ Gibson, Hamilton Bertie (1991). Hypnosis in therapy. Psychology Press. ISBN 978-0-86377-155-2.
- ^ a b Chen, Nancy N. (2003). "Chapter 4. Qiqong Deviation or Psychosis". Breathing spaces: qigong, psychiatry, and healing in China. Columbia University Press. pp. 77–107. ISBN 978-0-231-12804-9.
- ^ a b Liu, Tian Jun; Qiang, Xiao Mei, eds. (2013). Chinese Medical Qigong, Third Edition. Singing Dragon. ISBN 978-1848190962.
- ^ Liu, Lydia He (1999). Tokens of exchange: the problem of translation in global circulations. Durham, North Carolina: Duke University Press. p. 315. ISBN 978-0-8223-2424-9.
- ^ Shan, HH (2000). "Culture-bound psychiatric disorders associated with qigong practice in China" (PDF). Hong Kong J Psychiatry: 10–14.
- ^ The Chinese Society of Psychiatry (1989). "66. Qigong deviation syndrome". Chinese Classification and Diagnostic Criteria of Mental Disorders (CCMD-2). CCMD-2.
- ^ Human Rights Watch (2002). Dangerous minds: political psychiatry in China today and its origins in the Mao era. New York, New York: Human Rights Watch. ISBN 978-1-56432-278-4.
- ^ DSM-IV-TR, American Psychiatric Association, p. 902
- ^ Schatzberg, Alan F.; Hales, Robert E. (2008). American Psychiatric Publishing Textbook of Psychiatry. American Psychiatric Publishing, Inc. p. 1551. ISBN 978-1-58562-257-3.
- ^ Vuong, Ngan Kim (2006). "Cultural Bound Syndromes: Qigong Psychotic Reaction". In Jackson, Yo (ed.). Encyclopedia of Multicultural Psychology. SAGE Publications. pp. 142–143. ISBN 978-1-4129-0948-8.
- ^ Sandhu, Daya Singh (1999). Asian and Pacific Islander Americans : issues and concerns for counseling and psychotherapy. Commack, New York: Nova Science Publishers. p. 231. ISBN 978-1-56072-663-0.
- ^ Hwang, Wei-Chin (1 December 2007). "Qi-gong Psychotic Reaction in a Chinese American Woman". Culture, Medicine and Psychiatry. 31 (4): 547–560. doi:10.1007/s11013-007-9065-z. PMID 17932733. S2CID 31958321.
- ^ Robinson, Bruce H. (2007). Biomedicine: A Textbook for Practitioners of Acupuncture & Oriental Medicine. Blue Poppy Press. p. 434. ISBN 978-1-891845-38-3.
- ^ a b Robinson, Bruce H. (2007). Biomedicine: A Textbook for Practitioners of Acupuncture & Oriental Medicine. Blue Poppy Press. p. 435. ISBN 978-1-891845-38-3.
- ^ Lan, Fengli; Wallner, Friedrich G.; Wobovnik, Claudia (2011). Shen, psychotherapy, and acupuncture: theory, methodology, and structure of Chinese medicine. Culture and knowledge. Frankfurt am Main: P. Lang. ISBN 978-3-631-60762-6.
- ^ "国家体育总局健身气功管理中心". www.sport.gov.cn. Retrieved 2024-06-21.
- ^ Sing, Lee; Kleinman, Arthur (2002). "Psychiatry in its Political and Professional Contexts: A Response to Robin Munro" (PDF). J Am Acad Psychiatry Law. 30:120–5: 122.
- ^ "国家体育总局健身气功管理中心". www.sport.gov.cn. Retrieved 2024-06-21.
- ^ a b Xu, Xiangcai (2000). Qigong for Treating Common Ailments. YMAA Publication Center. ISBN 978-1-886969-70-4.
- ^ Ownby, David (2008). Falun Gong and the future of China. Oxford, England, UK: Oxford University Press. pp. 181–186. ISBN 978-0-19-532905-6. - Registration required
- ^ Ownby, David (2008-06-01), "Introduction", Falun Gong and the Future of China, Oxford University PressNew York, pp. 3–22, doi:10.1093/acprof:oso/9780195329056.003.0001, ISBN 0-19-532905-8, retrieved 2024-06-22