Flumequine[1] is a synthetic fluoroquinolone antibiotic[2][3] used to treat bacterial infections. It is a first-generation fluoroquinolone antibacterial that has been removed from clinical use and is no longer being marketed.[4] The marketing authorization of flumequine has been suspended throughout the EU.[5] It kills bacteria by interfering with the enzymes that cause DNA to unwind and duplicate. Flumequine was used in veterinarian medicine for the treatment of enteric infections (all infections of the intestinal tract),[6] as well as to treat cattle, swine, chickens, and fish, but only in a limited number of countries.[4][7][8] It was occasionally used in France (and a few other European Countries) to treat urinary tract infections under the trade name Apurone.[4][9] However this was a limited indication[10] because only minimal serum levels were achieved.[11]
 | |
| Clinical data | |
|---|---|
| Other names | 9-Fluoro-6,7-dihydro-5-methyl-1-oxo-1H,5H-benzo[ij]-quinolizine-2-carboxylic acid |
| AHFS/Drugs.com | International Drug Names |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Excretion | urine and feces |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.050.857 |
| Chemical and physical data | |
| Formula | C14H12FNO3 |
| Molar mass | 261.252 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 253 to 255 °C (487 to 491 °F) |
| |
| |
| | |
History
editThe first quinolone used was nalidixic acid (was marketed in many countries as Negram) followed by the fluoroquinolone flumequine.[4] The first-generation fluoroquinolone agents, such as flumequine, had poor distribution into the body tissues and limited activity. As such they were used mainly for treatment of urinary tract infections. Flumequine (benzo quinolizine) was first patented in 1973, (German Patent) by Rikker Labs.[12] Flumequine is a known antimicrobial compound described and claimed in U.S. Pat. No. 3,896,131 (Example 3), July 22, 1975.[13] Flumequine is the first quinolone compound with a fluorine atom at the C6-position of the related quinolone basic molecular structure.[14] Even though this was the first fluoroquinolone, it is often overlooked when classifying the drugs within this class by generations and excluded from such a list.
Though used frequently to treat farm animals and on occasion household pets, flumequine was also used to treat urinary tract infections in humans. Flumequine, was used transiently treat urinary infections[9] until ocular toxicity was reported.[15][16][17] as well as liver damage[18] and anaphylactic shock.[19][20]
In 2008, the United States Food and Drug Administration (FDA) requested that all quinolone/fluoroquinolone drugs package inserts include a Black Boxed Warning concerning the risk of spontaneous tendon ruptures, which would have included flumequine. The FDA also requested that the manufacturers send out Dear Doctor Letters regarding this new warning. Such tendon problems have also been associated with flumequine.[21]
Drug residue
editThe use of flumequine in food animals had sparked considerable debate. Significant and harmful residues of quinolones have been found in animals treated with quinolones and later slaughtered and sold as food products. There has been significant concern regarding the amount of flumequine residue found within food animals such as fish, poultry and cattle.[22][23] In 2003 the Joint FAO/WHO Committee on Food Additives (JECFA) withdrew the maximum residue limits (MRLs) for flumequine and carbadox based on evidence showing both are direct acting genotoxic carcinogens, therefore the Committee was unable to establish an Acceptable Daily Intake (ADI) for human exposure to such residues.[24] Subsequently, in 2006, the JEFCA, re-established the ADI having received appropriate evidence and MRLs were re-specified. The role of JECFA is to evaluate toxicology, residue chemistry and related information and make recommendations for acceptable daily intake (ADI) levels and maximum residue limits (MRLs). At its 16th session, held May 2006, the Committee on Residues of Veterinary Drugs in Foods (CCRVDF) requested information on registered uses of flumequine. As the CCRVDF did not receive any information regarding the registered uses of flumequine that they had requested, the committee members agreed to discontinue work on the MRLs for flumequine in shrimp.[25][26]
Licensed uses
editUrinary tract infections (veterinary and human)[27]
Availability
editVeterinary use:
- Solution; Oral; 20% (prescription only)
- Solution; Oral; 10% (prescription only)
Human use:
- Tablet; Oral; Flumequine 400 mg (discontinued)
Mode of action
editFlumequine is a member of the quinolone antibiotics family, which are active against both Gram-positive and Gram-negative bacteria. It functions by inhibiting DNA gyrase, a type II topoisomerase, and topoisomerase IV,[28] enzymes necessary to separate bacterial DNA, thereby inhibiting cell division.
This mechanism can also affect mammalian cell replication. In particular, some congeners of this drug family (for example those that contain the C-8 fluorine),[29] display high activity not only against bacterial topoisomerases, but also against eukaryotic topoisomerases and are toxic to cultured mammalian cells and in vivo tumor models.[30]
Although quinolones are highly toxic to mammalian cells in culture, its mechanism of cytotoxic action is not known. Quinolone induced DNA damage was first reported in 1986 (Hussy et al.).[31]
Recent studies have demonstrated a correlation between mammalian cell cytotoxicity of the quinolones and the induction of micronuclei.[32][33][34][35]
As such, some fluoroquinolones may cause injury to the chromosome of eukaryotic cells.[36][37][38][39][40][41]
There continues to be considerable debate as to whether or not this DNA damage is to be considered one of the mechanisms of action concerning the severe adverse reactions experienced by some patients following fluoroquinolone therapy.[30][42]
Adverse reactions
editFlumequine was associated with severe ocular toxicity, which precluded its use in human patients.[15][16][17] Drug-induced calculi (kidney stones) has been associated with such therapy as well.[43][44][45] Anaphylactic shock induced by flumequine therapy has also been associated with its use.[19][20][46] Anaphylactoid reactions such as shock, urticaria, and Quincke’s oedema have been reported to generally appear within two hours after taking the first tablet. There were eighteen reports listed within the WHO file in 1996.[47] As with all drugs within this class, flumequine therapy may result in severe central nervous system (CNS) reactions,[48][49][50] phototoxicity resulting in skin reactions like erythema, pruritus, urticaria and severe rashes,[51][52] gastrointestinal and neurological disorders.[9]
Drug interactions
editFlumequine was found to have no effect on theophylline pharmacokinetics.[53]
Chemistry
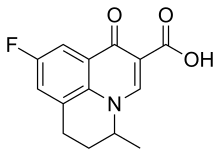
editFlumequine is a 9-fluoro-6,7-dihydro-5-methyl-1-oxo-1H,5H-benzo[ij]quinolizine-2-carboxylic acid. The molecular formula is C14H12FNO3. It is a white powder, odorless, flavorless, insoluble in water but soluble in organic solvent.[54]
Pharmacokinetics
editFlumequine is considered to be well absorbed and is excreted in the urine and feces as the glucuronide conjugates of the parent drug and 7-hydroxyflumequine. It is eliminated within 168 hours post-dosing. However, studies concerning the calf liver showed additional unidentified residues, of which a new metabolite, ml, represented the major single metabolite 24 hours after the last dose and at all subsequent time points. The metabolite ml, which exhibited no antimicrobial activity, was present in both free and protein-bound fractions. The major residue found in the edible tissues of sheep, pigs, and chickens was parent drug together with minor amounts of the 7-hydroxy-metabolite. The only detected residue in trout was the parent drug.[55]
See also
editReferences
edit- ^ INN: Lomefloxacin Hydrochloride
- ^ Nelson JM, Chiller TM, Powers JH, Angulo FJ (April 2007). "Fluoroquinolone-resistant Campylobacter species and the withdrawal of fluoroquinolones from use in poultry: a public health success story". Clinical Infectious Diseases. 44 (7): 977–980. doi:10.1086/512369. PMID 17342653.
- ^ Kawahara S (December 1998). "[Chemotherapeutic agents under study]". Nihon Rinsho. Japanese Journal of Clinical Medicine (in Japanese). 56 (12): 3096–3099. PMID 9883617.
- ^ a b c d "Quinolones and fluoroquinolones". Pharmacorama. Archived from the original on 2019-05-12. Retrieved 2010-04-04.
- ^ "Disabling and potentially permanent side effects lead to suspension or restrictions of quinolone and fluoroquinolone antibiotics". European Medicines Agency. 11 March 2019.
- ^ Francis PG, Wells RJ (1998). "Flumequine". Joint FAO/WHO Expert Committee on Food Additives. Residues of some veterinary drugs in animals and foods. Rome: Food and Agriculture Organization. ISBN 92-5-104128-8. OCLC 39798999.
- ^ Use of quinolones in food animals and potential impact on human health (PDF). WHO meeting. Geneva, Switzerland: World Health Organization. June 1998. Archived from the original (PDF) on 14 January 2010. Cattle only in Europe and Latin America. (Limited use in Latin America), Poultry only in Europe, Asia and Latin America, Fish only in Asia
- ^ Lavenberg DL. "IX4Q 4586, Brrytrit 3.23% Concentrate Solution for Use in Chicken Drinking Water, Genera. Correspondence, Published Literure" (PDF). Bayer. Archived from the original (PDF) on 5 October 2012 – via U.S. Food and Drug Administration.
Quinalones are often used to treat severe cases of human infection with Campylobacter spp., and they are also used in veterinary medicine, especially for treating poultry.
- ^ a b c Schena FP, Gesualdo L, Caracciolo G (January 1988). "A multicentre study of flumequine in the treatment of urinary tract infections". The Journal of Antimicrobial Chemotherapy. 21 (1): 101–106. doi:10.1093/jac/21.1.101. PMID 3356617.
- ^ The quinolones (Third Edition 2000) By Vincent T. Andriole Chapter I History and overview By Dr. Peter Ball (page 5)
- ^ King DE, Malone R, Lilley SH (May 2000). "New classification and update on the quinolone antibiotics". American Family Physician. 61 (9): 2741–2748. PMID 10821154.
- ^ "Generics (UK) Ltd v Daiichi Pharmaceutical Co Ltd". Reports of Patent, Design and Trade Mark Cases. 126 (2): 102. 2009. doi:10.1093/rpc/rcn037.
- ^ "Substituted benzo(ij)quinolizine-2-carboxylic acids and derivatives thereof - Patent 3896131". Freepatentsonline.com. Retrieved 2010-04-04.
- ^ Takahashi H, Hayakawa I, Akimoto T (2003). "[The history of the development and changes of quinolone antibacterial agents]". Yakushigaku Zasshi (in Japanese). 38 (2): 161–179. PMID 15143768.
- ^ a b Sirbat D, Saudax E, Hurault de Ligny B, Hachet E, Abellan P, George JL (1983). "[Serous macular detachment and treatment with flumequine (Apurone = urinary antibacterial). Apropos of 2 cases]". Bulletin des Sociétés d'Ophtalmologie de France (in French). 83 (8–9): 1019–1021. PMID 6378414.
- ^ a b Hurault de Ligny B, Sirbat D, Kessler M, Trechot P, Chanliau J (1984). "[Ocular side effects of flumequine. 3 cases of macular involvement]". Therapie (in French). 39 (5): 595–600. PMID 6506018.
- ^ a b Ball P (July 2000). "Quinolone generations: natural history or natural selection?". The Journal of Antimicrobial Chemotherapy. 46 (Suppl T1): 17–24. doi:10.1093/oxfordjournals.jac.a020889. PMID 10997595.
- ^ Dubois A, Janbon C, Pignodel C, Marty-Double C (February 1983). "[Immunoallergic hepatitis induced by flumequine]". Gastroenterologie Clinique et Biologique (in French). 7 (2): 217–218. PMID 6840466.
- ^ a b Pinzani V, Gennaro G, Petit P, Blayac JP (1992). "[Anaphylactic shock induced by flumequine]". Therapie (in French). 47 (5): 440. PMID 1299991.
- ^ a b Marsepoil T, Blin F, Lo JM, Horel D'Ancona F, Sebbah JL (September 1985). "[A case of anaphylactic shock induced by flumequine]". Presse Médicale (in French). 14 (32): 1712. PMID 2932732.
- ^ "Fluoroquinolones- A Review– Dr.T R RAMANUJAM.M.D". Medindia.net. Retrieved 2010-04-04.
- ^ Karbiwnyk CM, Hibbard LE, Lee RH, et al. (April 27–28, 2005). Confirmation of Oxolinic Acid and Flumequine Residues in Shrimp by Liquid Chromatography with Tandem Mass Spectrometry Detection. FDA Science.
- ^ "Chemotherapeutics in Seafood Compliance Program: Chapter 4: Pesticides and Chemical Contaminants" (PDF). Compliance Program Guidance Manual. U.S. Food and Drug Administration. 7304.018. Archived from the original (PDF) on 7 March 2011.
Residue found in Catfish/Basa, Shrimp, salmon, trout
- ^ "FAO/WHO Expert Committee on Food Additives, Geneva, Switzerland". Fda.gov. 2009-10-28. Retrieved 2010-04-04.
- ^ "FDA Veterinarian Newsletter, Volume XXII, No. V, 2007" (PDF). Food and Drug Administration. Retrieved 2010-04-04.
- ^ "Codex Committee on Veterinary Drug Residues Acts on Several Documents at 17th Session". Fda.gov. 2009-10-28. Retrieved 2010-04-04.
- ^ WHO Drug Information Vol. 2, No. 3, 1988
- ^ Drlica K, Zhao X (September 1997). "DNA gyrase, topoisomerase IV, and the 4-quinolones". Microbiology and Molecular Biology Reviews. 61 (3): 377–392. doi:10.1128/mmbr.61.3.377-392.1997. PMC 232616. PMID 9293187.
- ^ Robinson MJ, Martin BA, Gootz TD, McGuirk PR, Osheroff N (April 1992). "Effects of novel fluoroquinolones on the catalytic activities of eukaryotic topoisomerase II: Influence of the C-8 fluorine group". Antimicrobial Agents and Chemotherapy. 36 (4): 751–756. doi:10.1128/aac.36.4.751. PMC 189387. PMID 1323952.
- ^ a b Sissi C, Palumbo M (November 2003). "The quinolone family: from antibacterial to anticancer agents". Current Medicinal Chemistry. Anti-Cancer Agents. 3 (6): 439–450. doi:10.2174/1568011033482279. PMID 14529452.
The present review focuses on the structural modifications responsible for the transformation of an antibacterial into an anticancer agent. Indeed, a distinctive feature of drugs based on the quinolone structure is their remarkable ability to target different type II topoisomerase enzymes. In particular, some congeners of this drug family display high activity not only against bacterial topoisomerases but also against eukaryotic topoisomerases and are toxic to cultured mammalian cells and in vivo tumor models
- ^ Hussy P, Maass G, Tümmler B, Grosse F, Schomburg U (June 1986). "Effect of 4-quinolones and novobiocin on calf thymus DNA polymerase alpha primase complex, topoisomerases I and II, and growth of mammalian lymphoblasts". Antimicrobial Agents and Chemotherapy. 29 (6): 1073–1078. doi:10.1128/AAC.29.6.1073. PMC 180502. PMID 3015015.
- ^ Hosomi J, Maeda A, Oomori Y, Irikura T, Yokota T (1988). "Mutagenicity of Norfloxacin and AM-833 in Bacteria and Mammalian Cells". Reviews of Infectious Diseases. 10 (Supplement 1): S148–9. JSTOR 4454399.
- ^ Forsgren A, Bredberg A, Pardee AB, Schlossman SF, Tedder TF (May 1987). "Effects of ciprofloxacin on eucaryotic pyrimidine nucleotide biosynthesis and cell growth". Antimicrobial Agents and Chemotherapy. 31 (5): 774–779. doi:10.1128/AAC.31.5.774. PMC 174831. PMID 3606077.
- ^ Gootz TD, Barrett JF, Sutcliffe JA (January 1990). "Inhibitory effects of quinolone antibacterial agents on eucaryotic topoisomerases and related test systems". Antimicrobial Agents and Chemotherapy. 34 (1): 8–12. doi:10.1128/AAC.34.1.8. PMC 171510. PMID 2158274.
- ^ Lawrence JW, Darkin-Rattray S, Xie F, Neims AH, Rowe TC (February 1993). "4-Quinolones cause a selective loss of mitochondrial DNA from mouse L1210 leukemia cells". Journal of Cellular Biochemistry. 51 (2): 165–174. doi:10.1002/jcb.240510208. PMID 8440750. S2CID 41291987.
- ^ Elsea SH, Osheroff N, Nitiss JL (July 1992). "Cytotoxicity of quinolones toward eukaryotic cells. Identification of topoisomerase II as the primary cellular target for the quinolone CP-115,953 in yeast". The Journal of Biological Chemistry. 267 (19): 13150–13153. doi:10.1016/S0021-9258(18)42185-0. PMID 1320012.
- ^ Suto MJ, Domagala JM, Roland GE, Mailloux GB, Cohen MA (December 1992). "Fluoroquinolones: relationships between structural variations, mammalian cell cytotoxicity, and antimicrobial activity". Journal of Medicinal Chemistry. 35 (25): 4745–4750. doi:10.1021/jm00103a013. PMID 1469702.
- ^ Enzmann H, Wiemann C, Ahr HJ, Schlüter G (April 1999). "Damage to mitochondrial DNA induced by the quinolone Bay y 3118 in embryonic turkey liver". Mutation Research. 425 (2): 213–224. doi:10.1016/S0027-5107(99)00044-5. PMID 10216214.
- ^ Kashida Y, Sasaki YF, Ohsawa K, Yokohama N, Takahashi A, Watanabe T, Mitsumori K (October 2002). "Mechanistic study on flumequine hepatocarcinogenicity focusing on DNA damage in mice". Toxicological Sciences. 69 (2): 317–321. doi:10.1093/toxsci/69.2.317. PMID 12377980.
- ^ Thomas A, Tocher J, Edwards DI (May 1990). "Electrochemical characteristics of five quinolone drugs and their effect on DNA damage and repair in Escherichia coli". The Journal of Antimicrobial Chemotherapy. 25 (5): 733–744. doi:10.1093/jac/25.5.733. PMID 2165050.
- ^ "Fluoroquinolones and Quinolones". The American Academy of Optometry (British Chapter). Retrieved 29 January 2009.
- ^ Al-Soud YA, Al-Masoudi NA (2003). "A new class of dihaloquinolones bearing N'-aldehydoglycosylhydrazides, mercapto-1,2,4-triazole, oxadiazoline and a-amino ester precursors: synthesis and antimicrobial activity". Journal of the Brazilian Chemical Society. 14 (5): 790–796. doi:10.1590/S0103-50532003000500014.
- ^ Daudon M, Protat MF, Réveillaud RJ (1983). "[Detection and diagnosis of drug induced lithiasis]". Annales de Biologie Clinique (in French). 41 (4): 239–249. PMID 6139048.
- ^ Rincé C, Daudon M, Moesch C, Rincé M, Leroux-Robert C (May 1987). "Identification of flumequine in a urinary calculus". Journal of Clinical Chemistry and Clinical Biochemistry. 25 (5): 313–314. PMID 3612030.
- ^ Reveillaud RJ, Daudon M (October 1983). "[Drug-induced urinary lithiasis]". Presse Médicale (in French). 12 (38): 2389–2392. PMID 6138768.
- ^ Arboit F, Bessot JC, DeBlay F, Dietemann A, Charpentier C, Pauli G (January 1997). "Eight cases of quinolone allergy". Revue Française d'Allergologie et d'Immunologie Clinique. 37 (1): 15–19. doi:10.1016/S0335-7457(97)80204-3.
- ^ Adverse Reaction Newsletter 1996:1 Archived 2012-02-19 at the Wayback Machine WHO collaborating centre for international drug monitoring
- ^ Christ W (October 1990). "Central nervous system toxicity of quinolones: human and animal findings". The Journal of Antimicrobial Chemotherapy. 26 (Suppl B): 219–225. doi:10.1093/jac/26.suppl_b.219. PMID 2124211.
- ^ Defoin JF, Debonne T, Rambourg MO, Seraphin J, Buffet M, Jaussaud M, et al. (1990). "[Acute psychiatric syndrome and quinolones]". Journal de Toxicologie Clinique et Expérimentale (in French). 10 (7–8): 469–472. PMID 2135062.
- ^ Rampa S, Caroli F (1991). "[Neuropsychiatric manifestations and quinolones. Apropos of a case]". L'Encephale (in French). 17 (6): 511–514. PMID 1666873.
- ^ Vermeersch G, Filali A, Marko J, Catteau JP, Couture A (1990). "[Photophysical evaluation of photosensitization by various quinolones]". Journal de Pharmacie de Belgique (in French). 45 (5): 299–305. PMID 1964964.
- ^ Revuz J, Pouget F (1983). "[Photo-onycholysis caused by Apurone]". Annales de Dermatologie et de Venereologie (in French). 110 (9): 765. PMID 6660786.
- ^ Lacarelle B, Blin O, Audebert C, Auquier P, Karsenty H, Horriere F, Durand A (1994). "The quinolone, flumequine, has no effect on theophylline pharmacokinetics". European Journal of Clinical Pharmacology. 46 (5): 477–478. doi:10.1007/bf00191915. PMID 7957547. S2CID 97621.
- ^ "Flumequine(antiniotic antimicrobial agents) Manufacturers & Suppliers". 88chem.com. Retrieved 2010-04-04.
- ^ Francis PG, Wells RJ. "Flumequine". Pymble, Australia: Australian Government Analytical Laboratories.