Guanidinoacetate methyltransferase deficiency (GAMT deficiency) is an autosomal recessive[1] cerebral creatine deficiency that primarily affects the nervous system and muscles. It is the first described disorder of creatine metabolism, and results from deficient activity of guanidinoacetate methyltransferase, an enzyme involved in the synthesis of creatine.[2] Clinically, affected individuals often present with hypotonia, seizures and developmental delay. Diagnosis can be suspected on clinical findings, and confirmed by specific biochemical tests, brain magnetic resonance spectroscopy, or genetic testing. Biallelic pathogenic variants in GAMT are the underlying cause of the disorder. After GAMT deficiency is diagnosed, it can be treated by dietary adjustments, including supplementation with creatine. Treatment is highly effective if started early in life. If treatment is started late, it cannot reverse brain damage which has already taken place.
| Guanidinoacetate methyltransferase deficiency | |
|---|---|
| Other names | GAMT deficiency |
 | |
| Specialty | Medical genetics |
| Causes | Deficiency of guanidinoacetate methyltransferase enzyme |
| Diagnostic method | Genetic testing, magnetic resonance spectroscopy, blood and urine testing |
| Treatment | Dietary adjustment and creatine supplementation |
Signs and symptoms
editIndividuals with GAMT deficiency appear normal at birth. Shortly after birth, infants may start to show signs, as the consequences of decreased creatine levels in their body become more apparent. These clinical findings are relatively non-specific, and do not immediately suggest a disorder of creatine metabolism. Common clinical findings, as with other cerebral creatine deficiencies, include developmental delay (both intellectual and motor), seizures and hypotonia.[3][4] Speech delay, autism, and self-injurious behaviour have also been described.[5]
Genetics
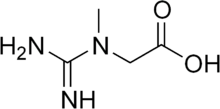
editBiallelic pathogenic variants in GAMT are associated with guanidinoacetate methyltransferase deficiency. This gene codes for the enzyme guanidinoacetate methyltransferase (GAMT), which participates in the two-step synthesis of the compound creatine from amino acids glycine, arginine and methionine. Specifically, GAMT controls the second step of the sequence, in which creatine is produced from another compound called guanidinoacetate.[6] The effects of GAMT deficiency are most severe in organs and tissues that require large amounts of energy, such as the brain and muscles.[citation needed]
This disorder is inherited in an autosomal recessive manner, which means the causative gene is located on an autosome, and two defective copies of the gene – one from each parent – are required to inherit the disorder. The parents both carry one pathogenic variant, however they are not affected by the disorder. As carriers, the residual activity of approximately 50% is enough to avoid clinical complications.[3] Any siblings of an GAMT deficient individual have a 25% chance of also being GAMT deficient, a 50% chance of being an asymptomatic carrier, and a 25% chance of being unaffected and not a carrier.[7]
Diagnosis
editGAMT deficiency can be suspected from clinical findings, although clinical findings are not suggestive of a specific diagnosis. Laboratory testing of plasma and urine will show decreased levels of creatine and increased levels of guanidinoacetate. Non-specific elevations of metabolites on urine testing, such as organic acid analysis, that are normalized to creatinine may be observed. For these tests, the excretion of urine metabolites is not elevated, but appears elevated due to unusually low creatinine values.[4] Specific diagnostic testing for GAMT deficiency relies on the measurement of guanidinoacetate and creatine in urine and plasma. Increased levels of guanidinoacetate and decreased levels of creatine can suggest a diagnosis.[4] Confirmatory testing can include enzyme assays to directly measure guanidinoacetate methyltransferase activity or molecular testing of GAMT. Brain magnetic resonance spectroscopy will show decreased levels of creatine, in affected individuals, however this finding is seen in all three cerebral creatine deficiencies, and needs to be followed up to identify the specific defect.[4]
Treatment is most effective for GAMT deficiency with early diagnosis, however the non-specific clinical findings mean there is often a delay in diagnosis. Due to the efficacy of treatment and the delay in diagnosis, GAMT deficiency has been recommended for newborn screening by the United States Advisory Committee on Heritable Disorders in Newborns and Children. Newborn screening assays measure the amount of guanidinoacetate in a dried blood spot using tandem mass spectrometry. Abnormal results from a newborn screening test still need to be confirmed by testing in plasma or urine.[8]
GAMT deficiency was nominated to be included in the list of disorders recommended for screening in the United States in 2016. It was initially not recommended for inclusion, as studies completed at the time could not demonstrate that a case could be reliably identified in a newborn screening setting.[9] Utah started screening for GAMT deficiency in all newborns in 2015. New York started screening newborns in late 2018.[10] In 2020, a GAMT-positive infant was identified via newborn screening in Utah,[11] thus providing evidence that a case could be identified from newborn screening. A second infant was identified in New York in 2021.[11] In 2022, a federal advisory committee voted to include GAMT in the Recommended Universal Screening Panel starting in January 2023.[12] California began screening for GAMT in 2024.[13]
Treatment
editTreatment of GAMT deficiency focuses on restoration of depleted brain creatine with creatine supplementation in pharmacologic doses, and removal of toxic intermediates via ornithine supplementation.[9] All patients are reported to benefit by this treatment, with improvements in muscular hypotonia, dyskinesia, social contact, alertness and behavior. Seizures appear to reduce more with dietary arginine restriction and ornithine supplementation. Despite treatment, none of the patients have been reported to return to completely normal developmental level, if significant damage had taken place before treatment. Prior to the addition of GAMT deficiency to newborn screening panels, younger siblings of affected individuals may have been tested at birth and treated early. This early treatment can result in outcomes that are very close to normal.[9]
References
edit- ^ Schulze, Andreas (2003). "Creatine deficiency syndromes". Molecular and Cellular Biochemistry. 244 (1/2): 143–150. doi:10.1023/A:1022443503883. ISSN 0300-8177. PMID 12701824. S2CID 25056424.
- ^ Stöckler, S; Isbrandt, D; Hanefeld, F; Schmidt, B; Von Figura, K (1 May 1996). "Guanidinoacetate methyltransferase deficiency: the first inborn error of creatine metabolism in man" (Free full text). American Journal of Human Genetics. 58 (5): 914–22. ISSN 0002-9297. PMC 1914613. PMID 8651275.
- ^ a b "612736 CEREBRAL CREATINE DEFICIENCY SYNDROME 2; CCDS2". Johns Hopkins University. Retrieved 2019-01-05.
- ^ a b c d Schulze, Andreas (2009). "Creatine Deficiency Syndromes". In Sarafoglou, Kiriakie; Hoffmann, Georg F.; Roth, Karl S. (eds.). Pediatric Endocrinology and Inborn Errors of Metabolism (1st ed.). New York: McGraw-Hill Medical. pp. 153–161. ISBN 978-0-07-143915-2.
- ^ Braissant, Olivier; Henry, Hugues; Béard, Elidie; Uldry, Joséphine (2011). "Creatine deficiency syndromes and the importance of creatine synthesis in the brain" (PDF). Amino Acids. 40 (5): 1315–1324. doi:10.1007/s00726-011-0852-z. ISSN 0939-4451. PMID 21390529. S2CID 13755292.
- ^ Clark, Joseph F.; Cecil, Kim M. (2014). "Diagnostic methods and recommendations for the cerebral creatine deficiency syndromes". Pediatric Research. 77 (3): 398–405. doi:10.1038/pr.2014.203. ISSN 0031-3998. PMID 25521922. S2CID 6720075.
- ^ Mercimek-Andrews, Saadet; Salomons, Gajja S. (1993), Adam, Margaret P.; Feldman, Jerry; Mirzaa, Ghayda M.; Pagon, Roberta A. (eds.), "Creatine Deficiency Disorders", GeneReviews®, Seattle (WA): University of Washington, Seattle, PMID 20301745, retrieved 2024-11-12
- ^ Ombrone D, Giocaliere E, Forni G, Malvagia S, la Marca G (2016). "Expanded newborn screening by mass spectrometry: New tests, future perspectives" (PDF). Mass Spectrom Rev. 35 (1): 71–84. Bibcode:2016MSRv...35...71O. doi:10.1002/mas.21463. hdl:2158/1010572. PMID 25952022. S2CID 21933819. Archived from the original (PDF) on 2022-03-29. Retrieved 2019-09-02.
- ^ a b c Chen, Daphne (2016-11-02). "Utah mom, doctors push to add rare disorder to national newborn screening panel". Deseret News, Utah. Archived from the original on November 3, 2016. Retrieved 2019-02-18.
- ^ "Newborn Screening Program". Association for Creatine Deficiencies. Retrieved 2019-05-05.
- ^ a b Hart, Kim; Rohrwasser, Andreas; Wallis, Heidi; Golsan, Heather; Shao, Jianyin; Anderson, Taylor; Wang, Xiaoli; Szabo-Fresnais, Nicolas; Morrissey, Mark; Kay, Denise M.; Wojcik, Matthew; Galvin-Parton, Patricia A.; Longo, Nicola; Caggana, Michele; Pasquali, Marzia (2021-09-01). "Prospective identification by neonatal screening of patients with guanidinoacetate methyltransferase deficiency". Molecular Genetics and Metabolism. 134 (1): 60–64. doi:10.1016/j.ymgme.2021.07.012. ISSN 1096-7192.
- ^ Ream, Margie A.; Lam, Wendy K. K.; Grosse, Scott D.; Ojodu, Jelili; Jones, Elizabeth; Prosser, Lisa A.; Rose, Angela M.; Comeau, Anne Marie; Tanksley, Susan; Powell, Cynthia M.; Kemper, Alex R. (2023-08-01). "Evidence and Recommendation for Guanidinoacetate Methyltransferase Deficiency Newborn Screening". Pediatrics. 152 (2): e2023062100. doi:10.1542/peds.2023-062100. ISSN 1098-4275. PMC 10527896. PMID 37465909.
- ^ "NBS Program Disorders Detectable". www.cdph.ca.gov. Retrieved 2024-08-20.
Further reading
edit- National Library of Medicine. MedlinePlus - Guanidinoacetate methyltransferase deficiency
- GeneReview/NIH/UW entry on Cerebral Creatine Deficiency syndromes