Kwashiorkor (/ˌkwɒʃiˈɔːrkɔːr, -kər/ KWOSH-ee-OR-kor, -kər, is also KWASH-)[1] is a form of severe protein malnutrition characterized by edema and an enlarged liver with fatty infiltrates.[2] It is thought to be caused by sufficient calorie intake, but with insufficient protein consumption (or lack of good quality protein), which distinguishes it from marasmus. Recent studies have found that a lack of antioxidant micronutrients such as β-carotene, lycopene, other carotenoids, and vitamin C as well as the presence of aflatoxins may play a role in the development of the disease.[3] However, the exact cause of Kwashiorkor is still unknown. Inadequate food supply is correlated with occurrences of kwashiorkor; occurrences in high income countries are rare.[4] It occurs amongst weaning children to ages of about five years old.[2]
| Kwashiorkor | |
|---|---|
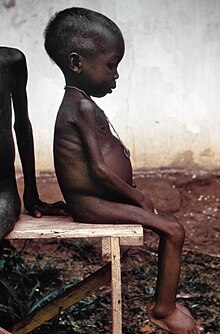 | |
| A young girl with kwashiorkor in a relief camp during the Nigerian Civil War | |
| Specialty | Pediatrics |
Conditions analogous to kwashiorkor were well documented around the world throughout history.[5] However, Jamaican pediatrician Cicely Williams introduced the term in 1935, two years after she published the disease's first formal description. Williams was the first to conduct research on kwashiorkor and differentiate it from other dietary deficiencies. She was the first to suggest that this might be a deficiency of protein.[6][7] The name is derived from the Ga language of coastal Ghana, translated as "the sickness the baby gets when the new baby comes" or "the disease of the deposed child", and reflecting the development of the condition in an older child who has been weaned from the breast when a younger sibling comes.[8] Breast milk contains amino acids vital to a child's growth. In at-risk populations, kwashiorkor may develop after children are weaned from breast milk and begin consuming a diet high in carbohydrates, including maize, cassava or rice.[2][6]
Classification
editKwashiorkor is a type of severe acute malnutrition (SAM). SAM is a category, composed of two conditions: marasmus and kwashiorkor.[9] Both kwashiorkor and marasmus fall under the umbrella of protein–energy malnutrition (PEM).[10] These diseases are oftentimes discussed together, but are distinctly separate conditions of malnutrition. Kwashiorkor is marked by an array of metabolic disturbances of uncertain etiology. In contrast, marasmus is more clearly a syndrome of energy deficiency, which is marked by weight loss. On physical exam, kwashiorkor is also distinguished from marasmus by the presence of edema. When children present with both kwashiorkor and marasmus, the condition is referred to as "marasmic-kwashiorkor".[11][3] In general, kwashiorkor is marked by more profound serum depletions of antioxidant molecules and minerals, relative to marasmus.[3]
Wellcome's classification
editWellcome classification[12] is a system for classifying protein-energy malnutrition in children based on weight for their age and based on presence of edema. Other classifications include Gomez classification and Waterlow classification.[13][14]
| Weight for age | With edema | Without edema | General considerations |
|---|---|---|---|
| 65-85% | Kwashiorkor | Undernutrition |
|
| <60% | Marasmic kwashiorkor | Marasmus |
Signs and symptoms
editThe defining sign of kwashiorkor in children is bilateral edema in the feet. Edema may also involve the hands, trunk, and face. Kwashiorkor is characterized by a fatty liver. This fatty liver of undernutrition phenotype is often accompanied by evidence of inflammation and fibrosis. Whereas a fatty liver of undernutrition is a consistent feature of kwashiorkor, it is only encountered sometimes in children with marasmus. In addition to this characteristic hepatic steatosis, kwashiorkor is marked by a parallel pattern of multi-organ dysfunction. Organs often affected in children with kwashiorkor include the kidneys, pancreas, heart, and nervous system.[3] Other findings that may be encountered on physical exam include a distended abdomen, hair thinning, loss of teeth, skin or hair depigmentation, and dermatitis. Children with kwashiorkor often develop irritability and anorexia. Generally, kwashiorkor is treated by introducing a high quality source of protein to the diet. Ready to use therapeutic food (RUTF) as well as F-100 and F-75 milk powders, which both include skim milk powder, are recommended for the treatment of kwashiorkor. These products are designed for use in low resource settings. The limited number of kwashiorkor cases that occur in high resource settings, where there is good access to advanced therapeutic tools, are typically treated with partially hydrolyzed or elemental enteral formulas, with parenteral nutrition provided in extreme cases.
Causes
editThe precise etiology of kwashiorkor remains unclear.[15][16][17] Several hypotheses have been proposed that are associated with and explain some, but not all aspects of the pathophysiology of kwashiorkor. They include, but are not limited to protein deficiency causing hypoalbuminemia, amino acid deficiency, oxidative stress, and gut microbiome changes.[15][17][18]
Low protein intake
editKwashiorkor is a severe form of malnutrition associated with a low protein diet.[2] The extreme lack of protein causes an osmotic imbalance in the gastrointestinal system causing swelling of the gut diagnosed as an edema or retention of water.[7]
Extreme fluid retention observed in individuals suffering from kwashiorkor is accompanied by irregularities in the lymphatic system as well as disruptions of capillary exchange. The lymphatic system serves three major purposes: fluid recovery, immunity, and lipid absorption. Victims of kwashiorkor commonly exhibit reduced ability to recover fluids, immune system failure, and low lipid absorption. Fluid recovery by the lymphatic system is accomplished by re-vascularization of fluid and macromolecules from the interstitial space, allowing these constituents of whole blood to be returned to the venous circulation. Compromised fluid recovery may contribute to the phenomenon of extravascular fluid accumulation in kwashiorkor.[20]
The low protein theory for the pathogenesis of kwashiorkor has been used to teach that capillary exchange between the lymphatic system and circulating blood is impaired by a reduced oncotic (i.e. colloid osmotic pressure, COP) in the blood, as a consequence of inadequate protein intake, so that the hydrostatic pressure gradient, which favors extravasation of fluid from small vessels, is not overcome. Proteins, mainly albumin, are responsible for creating the COP observed in the blood and tissue fluids. The difference in the COP of the blood and tissue tends to favor the reentry of fluid from the extravascular space, into the circulatory system. This tendency is opposed by the venous hydrostatic pressure, which tends to favor the exit of fluid from small vessels, into the interstitial space. The low protein theory for the pathogenesis of kwashiorkor held that a deficiency of serum proteins, caused by inadequate protein intake, disrupted this balance, and thus impaired the return flow of fluid from the interstitium into the capillary and venous structures. It has been taught that this is what accounts for the accumulation of extravascular fluid in kwashiorkor, and the subsequent pedal edema and abdominal distension.[21]
The low protein theory, which relies heavily upon Starling's theory for the movement of fluid in biological systems, provided a compelling rationale for the pathogenesis of edema in kwashiorkor. What it does not explain however, is the entire array of disturbances that define the kwashiorkor syndrome. These include, irritability, anorexia, skin desquamation, skin depigmentation, hair discoloration, reduced mitochondrial respiration, impaired lipid export from the liver without an accompanying reduction of lipoprotein synthesis, 'oxidative stress', glutathione depletions, transsulfuration disturbances, diffuse DNA hypomethylation, immune dysfunction, decreased transmethylation activity, and sulfated glycosaminoglycan deficiencies. It is now generally acknowledged that by itself, the low protein theory does not adequately account for the pathogenesis of kwashiorkor. More complex deficiencies are at work. These have still not been established. [22]
Social factors are also relevant. Ignorance of nutrition can be a cause. A case was described where parents who fed their child cassava failed to recognize malnutrition because of the edema caused by the syndrome and believed the child was well-nourished despite the development of kwashiorkor.[23]
Aflatoxins
editRecent studies have attempted to pinpoint a relationship between kwashiorkor and high levels of aflatoxins. Aflatoxins are naturally occurring toxins produced by the mold Aspergillus flavus, a fungus found in areas with hot and humid climates.[24] These toxins tend to grow and can be found in agricultural crops such as millet, maize, and rice.[24] An analysis found that the presence of aflatoxins was found more frequently and in higher concentrations in individuals with kwashiorkor when compared to individuals with marasmus (another form of severe acute malnutrition).[25][26] In particular, biological samples showed greater levels of aflatoxins in the brain, heart, kidney, liver, lungs, serum, stool, and urine.[25] Aflatoxins were not found in liver samples of individuals with marasmus.[25] It has been known that the liver organ is the main target of aflatoxins and chronic toxicity can result in immunosuppressive and carcinogenic effects.[25] However, there is currently conflicting evidence to pinpoint a connection between kwashiorkor and aflatoxins. Studies have shown that not all children with kwashiorkor present with detectable aflatoxin levels.[3] It has also been proposed that damage done by aflatoxins may be due to glutathione depletion (another proposed mechanism of the disease) in children with kwashiorkor.[3]
Mechanisms
editPeripheral edema and hypoalbuminemia
editKwashiorkor is a form of protein deficiency, which can result in both osmotic imbalances and irregularities in the lymphatic system.[3]
Kwashiorkor is most notable for peripheral edema. The presence of edema in kwashiorkor is correlated with very low albumin concentration (hypoalbuminemia). Edema results from a loss of fluid balance between the hydrostatic and oncotic pressures across the capillary blood vessel walls[2] due to the lack of protein which affects the body's ability to draw fluid from the tissues into the bloodstream. Low albumin concentration influences negatively the strength of oncotic pressure. Failure leads to the fluid buildup in the abdomen, resulting in edema and belly distension.[3]
Furthermore, the release of antidiuretic hormone is stimulated by hypovolemia, also leading to the development of peripheral edema. Plasma renin is also stimulated, promoting sodium retention.[2]
It is important to distinguish the pathophysiology of marasmus and kwashiorkor when it comes to treating malnourished children who may have hypovolemic shock that is cause by an acute loss of salt and water.[16] Children with severe albumin deficiency struggle physiologically to maintain their blood volume.[16]
Low glutathione levels
editKwashiorkor is also marked by low glutathione levels. Glutathione is used in many of the body processes on a molecule level.[27]
It is believed to be related to high oxidant levels commonly seen in people who suffer from starvation and rarely in chronic inflammation.[2] Glutathione serves vital functions including management of oxidative stress which is an imbalance that plays a key role in the pathogenesis of many diseases.
Evidence indicates that amino acid balance has an important effect on protein nutrition and therefore on glutathione homeostasis.[28]
Cysteine is an essential amino acid that acts as the limiting amino acid for glutathione synthesis in humans. Factors that increase demand for glutathione may increase demand for cysteine, and hence methionine. Such demands have been hypothesized to increase risk for kwashiorkor.
Others
editA proposed experimental theory suggests that alterations in the microbiome/virone contributes to edematous malnutrition, but further studies are required to understand the mechanism.[2]
Diagnosis
editKwashiorkor, or edematous malnutrition, like many other malnutrition diseases, is indirectly assessed using anthropometry.[9] Kwashiorkor is a subtype of severe acute malnutrition (SAM) characterized by bilateral peripheral pitting edema. According to the World Health Organization, the SAM diagnosis parameters are a "mid-upper arm circumference (MUAC) of < 115 mm, weight-for-height/length Z-score (WHZ) of < -3Z and nutritional edema or any combination of these parameters."[29][2][30] Additional clinical findings on physical exam include marked muscle atrophy, abdominal distension, dermatitis, and hepatomegaly.[2][31]
WHO criteria for clinical assessment of malnutrition are based on the degree of wasting (MUAC), stunting (weight-for-height Z-score), and the presence of edema (mild to severe).[32]
Screening
editBecause it can be difficult to measure weight-for-height Z scores (WHZ) frequently, screening is performed by physical exam, with careful examination of the child's feet to detect the presence of bilateral pitting edema. Screening for edema is essential for the diagnosis of kwashiorkor, since nearly two thirds of kwashiorkor cases do not have evidence of acute wasting (i.e. mid-upper arm circumference (MUAC) < 125 mm, or WHZ < -2) when diagnosed with kwashiorkor.
Prevention
editAs for the prevention of childhood malnutrition, there needs to be public health changes such as improving agriculture and improving access to healthcare to effectively reduce the rates of malnutrition in children. By educating individuals of childbearing age on proper nutrition and health during and after pregnancy, they can provide their children with the appropriate nutrients from a young age. By ensuring they are equipped with the proper education and resources, caretakers and infants are in better health, ultimately preventing childhood malnutrition.[9]
Because edema can hide decreased muscle mass, it can be hard to diagnose kwashiorkor in young children; however, if cases are overlooked, children become more susceptible to infections and can ultimately lead to morbidity and mortality.[33] To prevent this from happening, parents can be educated on proper nutrition and the importance of breastfeeding infants to ensure they receive all the nutrients they need.[33]
A diet rich in carbohydrates, fats that make up 10% of the total caloric needs, and proteins that make up 15% of the caloric needs can prevent kwashiorkor.
Proteins can be found in the following foods
- Seafood
- Peas
- Nuts
- Seeds
- Eggs
- Lean meat
- Beans[3]
Treatment
editWHO guidelines outline 10 general principles for the inpatient management of severely malnourished children.[32][34]
- Treat/prevent hypoglycemia
- Treat/prevent hypothermia
- Treat/prevent dehydration
- Correct electrolyte imbalance
- Treat/prevent infection
- Correct micronutrient deficiencies
- Start cautious feeding
- Achieve catch-up growth
- Provide sensory stimulation and emotional support
- Prepare for follow-up after recovery
Both clinical subtypes of severe acute malnutrition (kwashiorkor and marasmus) are treated similarly.[17][32] Upon initial treatment, children with kwashiorkor may experience weight loss as their edema resolves.[35] Therefore, after concerns of refeeding syndrome have passed, children may require 120-140% of their estimated caloric needs in order to achieve catch-up growth.[35]
The cause, type, and severity of malnutrition determines what type of treatment would be most appropriate.[36] For primary acute malnutrition, children with no complications are treated at home and are encouraged to either continue breastfeeding (for infants) or start using ready-to-use therapeutic foods (for children).[36] For secondary acute malnutrition, the underlying cause needs to be identified to appropriately treat children. Only after the primary disease is determined can an appropriate dietary plan be made, as fluid, vitamins, and macronutrients may need to be considered to not exacerbate the cause of the malnutrition.[36]
Ready-to-use therapeutic foods (RUTFs) and F-75 and F-100 milks were created to provide appropriate nutrition and caloric intake to those experiencing malnutrition. F-75 milk would be ideal when trying to reintroduce food into a malnourished person, and F-100 milk would be used to aid in weight gain. While RUTFs and F-100 milk were made to have the same nutritional value, RUTFs are beneficial as they are dehydrated and do not require much preparation.[9]
Prognosis
editKwashiorkor is associated with a high risk of mortality and long-term complications. Treatment under the guidelines of the World Health Organization has proven to reduce this mortality risk and affected children tend to recover faster than children with other severe malnutrition diseases. However, physical and intellectual capabilities are not fully restored. Growth stunting and chronic disruption of microbiota are commonly observed after recovery.[3]
A high risk of death is identified by a brachial perimeter < 11 cm or by a weight-for-age threshold < −3 z-scores below the median of the WHO child growth standards. In practice, malnourished children with edema are suffering from potentially life-threatening severe malnutrition.[37]
Epidemiology
editKwashiorkor is rare in high income countries. It is mostly observed in low-income and middle income nations and regions such as Southeast Asia, Central America, Congo, Ethiopia, Puerto Rico, Jamaica, South Africa, and Uganda, where poverty is prominent.[3] Occurrences of severe malnutrition also tend to trend higher under conditions of food insecurity, higher prevalence of infectious diseases, lack of access to appropriate care, and poor living situations with inadequate sanitation.[9] Communities experiencing famine are affected the most especially during the rainy season. Prevalence varies, but it affects children of either sex commonly under five years old.[3][10] "Globally, kwashiorkor indirected accounted for 53% of deaths among children under five between 2000 and 2003 when associated with other common childhood diseases like acute respiratory infections, malaria, measles, HIV/AIDS and other causes of perinatal deaths."[10]
When compared to marasmus in developing countries, kwashiorkor typically has a lower prevalence, "0.2%-1.6% for kwashiorkor and 1.2%-6.8% for marasmus."[3] Factors such as "diet, geographical locations, climate and aflatoxin exposure" have been invoked as potential causes for observed differences in the prevalence for kwashiorkor and marasmus.[3]
In general, in areas where Severe Acute Malnutrition (SAM) is prevalent, marasmus is more often the dominant SAM condition. However, in certain areas kwashiorkor may be more common than marasmus.
History
editKwashiorkor was present in the world long before 1933, when Cecily Williams published research which took the Ga name for the disease. There were already many names for the illness which referenced the cessation of breastfeeding, or the consumption of monotonous diets high in starch. However, Williams was the first to suggest that this might be a deficiency of protein or an amino acid. [7] [5] Despite publishing in 1933, it was only in 1949 that the World Health Organization officially recognized kwashiorkor as a public health concern.[2] This period also correlated with the promotion of infant formula, often by European colonial powers. The substitution of formula for breastmilk contributed significantly to the increasing visibility of kwashiorkor throughout the twentieth century. Cicely Williams later described the promotion of formula as "the most criminal form of sedition, and that those deaths should be regarded as murder." These arguments underpinned the 1970s Nestlé boycott.[5]
Effects on pharmacokinetics
editThose experiencing poverty-related infectious diseases (PRDs) such as malaria and tuberculosis are also likely to be malnourished.[38] Malnutrition can affect the pharmacokinetics of various drugs used to treat PRDs by changing a drug's bioavailability, distribution, and elimination.[38] To optimize treatment of those diseases, there needs to be more research into how severe malnutrition, specifically kwashiorkor, can affect treatment response.[38]
Research directions
editCurrent research and recommendations to manage severe acute malnutrition (SAM), such as kwashiorkor, in children are largely based on expert opinions. Only one-third of the WHO guidelines for management of SAM are based on epidemiological and clinical research. Further studies are needed in order to "improve treatment outcomes in the large number of children with SAM."[39]
See also
editReferences
edit- ^ Wells, John C. (2008). Longman Pronunciation Dictionary (3rd ed.). Longman. ISBN 978-1-4058-8118-0.
- ^ a b c d e f g h i j k Benjamin, Onecia; Lappin, Sarah L. (2022). "Kwashiorkor". StatPearls. StatPearls Publishing. PMID 29939653. NBK507876.
- ^ a b c d e f g h i j k l m n Pham, Thi-Phuong-Thao; Alou, Maryam Tidjani; Golden, Michael H.; Million, Matthieu; Raoult, Didier (January 2021). "Difference between kwashiorkor and marasmus: Comparative meta-analysis of pathogenic characteristics and implications for treatment". Microbial Pathogenesis. 150: 104702. doi:10.1016/j.micpath.2020.104702. PMID 33359074. S2CID 229694345. Archived from the original on 10 February 2023. Retrieved 9 February 2023.
- ^ Liu T, Howard RM, Mancini AJ, Weston WL, Paller AS, Drolet BA, et al. (2001). "Kwashiorkor in the United States: fad diets, perceived and true milk allergy, and nutritional ignorance". Archives of Dermatology. 137 (5): 630–6. PMID 11346341.[permanent dead link]
- ^ a b c Nott, John (May 2021). "'No one may starve in the British Empire': Kwashiorkor, Protein and the Politics of Nutrition Between Britain and Africa". Social History of Medicine. 34 (2): 553–576. doi:10.1093/shm/hkz107. PMC 8162845. PMID 34084092.
- ^ a b Williams CD (1983) [1933]. "Fifty years ago. Archives of Diseases in Childhood 1933. A nutritional disease of childhood associated with a maize diet". Archives of Disease in Childhood. 58 (7): 550–60. doi:10.1136/adc.58.7.550. PMC 1628206. PMID 6347092.
- ^ a b c Williams CD, Oxon BM, Lond H (1935). "Kwashiorkor: a nutritional disease of children associated with a maize diet. 1935". Bulletin of the World Health Organization. 81 (12): 912–3. doi:10.1016/S0140-6736(00)94666-X. PMC 2572388. PMID 14997245. Reprint: Williams CD, Oxon BM, Lond H (2003). "Kwashiorkor: a nutritional disease of children associated with a maize diet. 1935". Bulletin of the World Health Organization. 81 (12): 912–3. doi:10.1016/S0140-6736(00)94666-X. PMC 2572388. PMID 14997245.
- ^ Stanton, J. (2001). "Listening to the Ga: Cicely Williams' Discovery of Kwashiorkor on the Gold Coast" (PDF). Women and Modern Medicine. Clio Medica. Vol. 61. pp. 149–171. doi:10.1163/9789004333390_008. ISBN 978-90-04-33339-0. PMID 11603151. Archived (PDF) from the original on 1 December 2021. Retrieved 25 February 2022.
- ^ a b c d e Bhutta, Zulfiqar A.; Berkley, James A.; Bandsma, Robert H. J.; Kerac, Marko; Trehan, Indi; Briend, André (21 December 2017). "Severe childhood malnutrition". Nature Reviews Disease Primers. 3 (1): 17067. doi:10.1038/nrdp.2017.67. PMC 7004825. PMID 28933421.
- ^ a b c Odigwe, Chibuzo C; Smedslund, Geir; Ejemot-Nwadiaro, Regina I; Anyanechi, Chiedozie C; Krawinkel, Michael B (14 April 2010). "Supplementary vitamin E, selenium, cysteine and riboflavin for preventing kwashiorkor in preschool children in developing countries". Cochrane Database of Systematic Reviews. 2010 (4): CD008147. doi:10.1002/14651858.CD008147.pub2. PMC 6599860. PMID 20393967.
- ^ "Malnutrition (Kwashiorkor and Marasmus) — Symptoms and Treatment". The Lecturio Online Medical Library. 2017. Archived from the original on 27 October 2021. Retrieved 27 July 2021.
- ^ "Protein energy malnutrition classification - wikidoc". www.wikidoc.org. Archived from the original on 15 September 2022. Retrieved 29 July 2021.
- ^ Bender, David A., ed. (29 January 2009). "Wellcome classification". A Dictionary of Food and Nutrition. OUP Oxford. ISBN 978-0-19-157975-2. Archived from the original on 21 July 2022. Retrieved 30 July 2021.
- ^ Gernaat, H.; Voorhoeve, HW (1 April 2000). "A new classification of acute protein-energy malnutrition". Journal of Tropical Pediatrics. 46 (2): 97–106. doi:10.1093/tropej/46.2.97. PMID 10822936.
- ^ a b Briend A (2014). "Kwashiorkor: still an enigma – the search must go on" (PDF). Emergency Nutrition Network. Archived (PDF) from the original on 15 February 2022. Retrieved 2 August 2019.
- ^ a b c G. Coulthard, Malcolm (13 May 2015). "Oedema in kwashiorkor is caused by hypoalbuminaemia". Paediatrics and International Child Health. 35 (2): 83–89. doi:10.1179/2046905514Y.0000000154. PMC 4462841. PMID 25223408.
- ^ a b c Smith, Michelle I.; Yatsunenko, Tanya; Manary, Mark J.; Trehan, Indi; Mkakosya, Rajhab; Cheng, Jiye; Kau, Andrew L.; Rich, Stephen S.; Concannon, Patrick; Mychaleckyj, Josyf C.; Liu, Jie; Houpt, Eric; Li, Jia V.; Holmes, Elaine; Nicholson, Jeremy; Knights, Dan; Ursell, Luke K.; Knight, Rob; Gordon, Jeffrey I. (February 2013). "Gut Microbiomes of Malawian Twin Pairs Discordant for Kwashiorkor". Science. 339 (6119): 548–554. Bibcode:2013Sci...339..548S. doi:10.1126/science.1229000. PMC 3667500. PMID 23363771.
- ^ Velly H, Britton RA, Preidis GA (2017). "Mechanisms of cross-talk between the diet, the intestinal microbiome, and the undernourished host". Gut Microbes. 8 (2): 98–112. doi:10.1080/19490976.2016.1267888. PMC 5390823. PMID 27918230.
- ^ "Mortality and Burden of Disease Estimates for WHO Member States in 2002" (xls). World Health Organization. 2002. Archived from the original on 16 January 2013. Retrieved 5 October 2020.
- ^ "Nova et Vetera". The British Medical Journal. 2 (4673): 284. 1950. doi:10.1136/bmj.2.4673.267. S2CID 220181068.
- ^ Saladin K (2012). Anatomy and Physiology (6th ed.). New York: McGraw Hill. pp. 766–767, 809–811. ISBN 978-0-07-337825-1.
- ^ Tierney EP, Sage RJ, Shwayder T (2010). "Kwashiorkor from a severe dietary restriction in an 8-month infant in suburban Detroit, Michigan: case report and review of the literature". International Journal of Dermatology. 49 (5): 500–6. doi:10.1111/j.1365-4632.2010.04253.x. PMID 20534082. S2CID 13050691.
- ^ "Malnutrition in Third World Countries". www.religion-online.org. Archived from the original on 19 September 2015. Retrieved 2 March 2017.
- ^ a b Kumar, Pradeep; Mahato, Dipendra K.; Kamle, Madhu; Mohanta, Tapan K.; Kang, Sang G. (17 January 2017). "Aflatoxins: A Global Concern for Food Safety, Human Health and Their Management". Frontiers in Microbiology. 07: 2170. doi:10.3389/fmicb.2016.02170. PMC 5240007. PMID 28144235.
- ^ a b c d Soriano, Jose M.; Rubini, Ana; Morales-Suarez-Varela, María; Merino-Torres, Juan F.; Silvestre, Dolores (October 2020). "Aflatoxins in organs and biological samples from children affected by kwashiorkor, marasmus and marasmic-kwashiorkor: A scoping review". Toxicon. 185: 174–183. doi:10.1016/j.toxicon.2020.07.010. PMID 32693007. S2CID 220698925.
- ^ Watson, Sinead; Gong, Yun Yun; Routledge, Michael (15 July 2015). "Interventions Targeting Child Undernutrition in Developing Countries May Be Undermined by Dietary Exposure to Aflatoxin" (PDF). Critical Reviews in Food Science and Nutrition. 57 (9): 1963–1975. doi:10.1080/10408398.2015.1040869. PMID 26176888. S2CID 24089209.
- ^ Wu, Guoyo; Fang, Yun-Zhong; Yang, Sheng; Lupton, Joanne R; Turner, Nancy D. (2004). "Glutathione Metabolism and Its Implications for Health". The Journal of Nutrition. 134 (3): 489–492. doi:10.1093/jn/134.3.489. PMID 14988435. Archived from the original on 19 June 2022. Retrieved 29 July 2021.
- ^ Gould, Rebecca L.; Pazdro, Robert (11 May 2019). "Impact of Supplementary Amino Acids, Micronutrients, and Overall Diet on Glutathione Homeostasis". Nutrients. 11 (5): 1056. doi:10.3390/nu11051056. PMC 6566166. PMID 31083508.
- ^ Roberfroid, Dominique; Hammami, Naïma; Mehta, Pankti; Lachat, Carl; Verstraeten, Roosmarijn; Weise Prinzo, Zita; Huybregts, Lieven; Kolsteren, Patrick (2013). Management of oedematous malnutrition in infants and children aged >6 months: a systematic review of the evidence. CiteSeerX 10.1.1.655.6549. hdl:1854/LU-5700347.
- ^ Grellety, Emmanuel; Golden, Michael H. (December 2018). "Severely malnourished children with a low weight-for-height have similar mortality to those with a low mid-upper-arm-circumference: II. Systematic literature review and meta-analysis". Nutrition Journal. 17 (1): 80. doi:10.1186/s12937-018-0383-5. PMC 6138903. PMID 30217196.
- ^ Heilskov, S.; Rytter, M.J.H.; Vestergaard, C.; Briend, A.; Babirekere, E.; Deleuran, M.S. (August 2014). "Dermatosis in children with oedematous malnutrition (Kwashiorkor): a review of the literature". Journal of the European Academy of Dermatology and Venereology. 28 (8): 995–1001. doi:10.1111/jdv.12452. PMID 24661336. S2CID 24731334.
- ^ a b c Guideline: updates on the management of severe acute malnutrition in infants and children. World Health Organization. 2013. hdl:10665/95584. ISBN 978-92-4-150632-8.[page needed]
- ^ a b Kamaruzaman, NA; Jamani, NA; Said, AH (6 July 2020). "An infant with kwashiorkor: The forgotten disease". Malaysian Family Physician. 15 (2): 46–49. PMC 7430309. PMID 32843945.
- ^ Ashworth A (2003). "Guidelines for the inpatient treatment of severely malnourished children" (PDF). WHO. Archived from the original (PDF) on 27 March 2006.
- ^ a b Grover, Zubin; Ee, Looi C. (October 2009). "Protein Energy Malnutrition". Pediatric Clinics of North America. 56 (5): 1055–1068. doi:10.1016/j.pcl.2009.07.001. PMID 19931063.
- ^ a b c Dipasquale, Valeria; Cucinotta, Ugo; Romano, Claudio (12 August 2020). "Acute Malnutrition in Children: Pathophysiology, Clinical Effects and Treatment". Nutrients. 12 (8): 2413. doi:10.3390/nu12082413. PMC 7469063. PMID 32806622.
- ^ "Management of moderate malnutrition in under-5 children by the health sector" (PDF). Archived (PDF) from the original on 27 January 2018. Retrieved 6 May 2021.
- ^ a b c Verrest, Luka; Wilthagen, Erica A.; Beijnen, Jos H.; Huitema, Alwin D. R.; Dorlo, Thomas P. C. (September 2021). "Influence of Malnutrition on the Pharmacokinetics of Drugs Used in the Treatment of Poverty-Related Diseases: A Systematic Review". Clinical Pharmacokinetics. 60 (9): 1149–1169. doi:10.1007/s40262-021-01031-z. PMC 8545752. PMID 34060020. S2CID 235259789.
- ^ Kulkarni, Bharati; Mamidi, RajaSriswan (2019). "Nutrition rehabilitation of children with severe acute malnutrition: Revisiting studies undertaken by the National Institute of Nutrition". Indian Journal of Medical Research. 150 (2): 139–152. doi:10.4103/ijmr.IJMR_1905_18. PMC 6829782. PMID 31670269.
External links
edit- Picot, J; Hartwell, D; Harris, P; Mendes, D; Clegg, A J; Takeda, A (2012). "The effectiveness of interventions to treat severe acute malnutrition in young children: a systematic review". Health Technology Assessment. 16 (19): 1–316. doi:10.3310/hta16190. PMC 4781582. PMID 22480797. NBK98566.
- Media related to Kwashiorkor at Wikimedia Commons
- The dictionary definition of kwashiorkor at Wiktionary