Lisdexamfetamine, sold under the brand names Vyvanse and Elvanse among others, is a stimulant medication that is used to treat attention deficit hyperactivity disorder (ADHD) in children and adults and for moderate-to-severe binge eating disorder in adults.[15] Lisdexamfetamine is taken by mouth. Its effects generally begin within two hours and last for up to 14 hours.[15]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Vyvanse, Tyvense, Elvanse, others |
| Other names | L-Lysine-d-amphetamine; (2S)-2,6-Diamino-N-[(2S)-1-phenylpropan-2-yl]hexanamide N-[(2S)-1-Phenyl-2-propanyl]-L-lysinamide |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a607047 |
| License data | |
| Pregnancy category |
|
| Dependence liability | Moderate[1][2] |
| Addiction liability | Moderate[1][2] |
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | Oral: 96.4%[9] |
| Protein binding | 20% (as dextroamphetamine)[10] |
| Metabolism | Hydrolysis by enzymes in red blood cells initially, subsequent metabolism follows |
| Metabolites | Dextroamphetamine (and its metabolites) and L-lysine |
| Onset of action | Oral: <2 hours[11][12] |
| Elimination half-life | Lisdexamfetamine: <1 hour[13] Dextroamphetamine: 10–12 h[13][7] |
| Duration of action | 10–14 hours[14][11][12] |
| Excretion | Kidney: ~2% |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
| Formula | C15H25N3O |
| Molar mass | 263.385 g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Dextrorotatory enantiomer |
| |
| |
| | |
Common side effects of lisdexamfetamine include loss of appetite, anxiety, diarrhea, trouble sleeping, irritability, and nausea.[15] Rare but serious side effects include mania, sudden cardiac death in those with underlying heart problems, and psychosis.[15] It has a high potential for substance abuse.[7][15] Serotonin syndrome may occur if used with certain other medications.[15] Its use during pregnancy may result in harm to the baby and use during breastfeeding is not recommended by the manufacturer.[16][15][17]
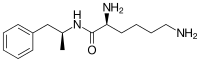
Lisdexamfetamine is an inactive prodrug that works after being converted by the body into dextroamphetamine, a central nervous system (CNS) stimulant.[15][18] Chemically, lisdexamfetamine is composed of the amino acid L-lysine, attached to dextroamphetamine.[19]
Lisdexamfetamine was approved for medical use in the United States in 2007, and in the European Union in 2012.[15][20] In 2022, it was the 69th most commonly prescribed medication in the United States, with more than 9 million prescriptions.[21][22] It is a Class B controlled substance in the United Kingdom, a Schedule 8 controlled drug in Australia, and a Schedule II controlled substance in the United States.[16][23]
Uses
editMedical
editLisdexamfetamine is used primarily as a treatment for attention deficit hyperactivity disorder (ADHD) and binge eating disorder;[7] it has similar off-label uses as those of other pharmaceutical amphetamines.[14] Individuals over the age of 65 were not commonly tested in clinical trials of lisdexamfetamine for ADHD.[7] According to a 2019 systematic review, lisdexamfetamine was the most effective treatment for adult ADHD.[24]
ADHD
editLong-term amphetamine exposure at sufficiently high doses in some animal species is known to produce abnormal dopamine system development or nerve damage,[25][26] but, in humans with ADHD, long-term use of pharmaceutical amphetamines at therapeutic doses appears to improve brain development and nerve growth.[27][28][29] Reviews of magnetic resonance imaging (MRI) studies suggest that long-term treatment with amphetamine decreases abnormalities in brain structure and function found in subjects with ADHD, and improves function in several parts of the brain, such as the right caudate nucleus of the basal ganglia.[27][28][29]
Reviews of clinical stimulant research have established the safety and effectiveness of long-term continuous amphetamine use for the treatment of ADHD.[30][31][32] Randomized controlled trials of continuous stimulant therapy for the treatment of ADHD spanning 2 years have demonstrated treatment effectiveness and safety.[30][31] Two reviews have indicated that long-term continuous stimulant therapy for ADHD is effective for reducing the core symptoms of ADHD (i.e., hyperactivity, inattention, and impulsivity), enhancing quality of life and academic achievement, and producing improvements in a large number of functional outcomes[note 1] across 9 categories of outcomes related to academics, antisocial behavior, driving, non-medicinal drug use, obesity, occupation, self-esteem, service use (i.e., academic, occupational, health, financial, and legal services), and social function.[30][32] One review highlighted a nine-month randomized controlled trial of amphetamine treatment for ADHD in children that found an average increase of 4.5 IQ points, continued increases in attention, and continued decreases in disruptive behaviors and hyperactivity.[31] Another review indicated that, based upon the longest follow-up studies conducted to date, lifetime stimulant therapy that begins during childhood is continuously effective for controlling ADHD symptoms and reduces the risk of developing a substance use disorder as an adult.[30]
Current models of ADHD suggest that it is associated with functional impairments in some of the brain's neurotransmitter systems;[33] these functional impairments involve impaired dopamine neurotransmission in the mesocorticolimbic projection and norepinephrine neurotransmission in the noradrenergic projections from the locus coeruleus to the prefrontal cortex.[33] Stimulants like methylphenidate and amphetamine are effective in treating ADHD because they increase neurotransmitter activity in these systems.[34][33][35] Approximately 80% of those who use these stimulants see improvements in ADHD symptoms.[36] Children with ADHD who use stimulant medications generally have better relationships with peers and family members, perform better in school, are less distractible and impulsive, and have longer attention spans.[37][38] The Cochrane reviews[note 2] on the treatment of ADHD in children, adolescents, and adults with pharmaceutical amphetamines stated that short-term studies have demonstrated that these drugs decrease the severity of symptoms, but they have higher discontinuation rates than non-stimulant medications due to their adverse side effects.[40][41] A Cochrane review on the treatment of ADHD in children with tic disorders such as Tourette syndrome indicated that stimulants in general do not make tics worse, but high doses of dextroamphetamine could exacerbate tics in some individuals.[42]
Binge Eating Disorder
editBinge eating disorder (BED) is characterized by recurrent and persistent episodes of compulsive binge eating.[43] These episodes are often accompanied by marked distress and a feeling of loss of control over eating.[43] The pathophysiology of BED is not fully understood, but it is believed to involve dysfunctional dopaminergic reward circuitry along the cortico-striatal-thalamic-cortical loop.[44][45] As of July 2024, lisdexamfetamine is the only USFDA- and TGA-approved pharmacotherapy for BED.[46][47] Evidence suggests that lisdexamfetamine's treatment efficacy in BED is underpinned at least in part by a psychopathological overlap between BED and ADHD, with the latter conceptualized as a cognitive control disorder that also benefits from treatment with lisdexamfetamine.[44][45]
Lisdexamfetamine's therapeutic effects for BED primarily involve direct action in the central nervous system after conversion to its pharmacologically active metabolite, dextroamphetamine.[47] Centrally, dextroamphetamine increases neurotransmitter activity of dopamine and norepinephrine in prefrontal cortical regions that regulate cognitive control of behavior.[44][47] Similar to its therapeutic effect in ADHD, dextroamphetamine enhances cognitive control and may reduce impulsivity in patients with BED by enhancing the cognitive processes responsible for overriding prepotent feeding responses that precede binge eating episodes.[44][49][50] In addition, dextroamphetamine's actions outside of the central nervous system may also contribute to its treatment effects in BED. Peripherally, dextroamphetamine triggers lipolysis through noradrenergic signaling in adipose fat cells, leading to the release of triglycerides into blood plasma to be utilized as a fuel substrate.[45][51] Dextroamphetamine also activates TAAR1 in peripheral organs along the gastrointestinal tract that are involved in the regulation of food intake and body weight.[48] Together, these actions confer an anorexigenic effect that promotes satiety in response to feeding and may decrease binge eating as a secondary effect.[50][48]
Medical reviews of randomized controlled trials have demonstrated that lisdexamfetamine, at doses between 50-70 mg, is safe and effective for the treatment of moderate-to-severe BED in adults.[sources 1] These reviews suggest that lisdexamfetamine is persistently effective at treating BED and is associated with significant reductions in the number of binge eating days and binge eating episodes per week.[sources 1] Furthermore, a meta-analytic systematic review highlighted an open-label, 12-month extension safety and tolerability study that reported lisdexamfetamine remained effective at reducing the number of binge eating days for the duration of the study.[50] In addition, both a review and a meta-analytic systematic review found lisdexamfetamine to be superior to placebo in several secondary outcome measures, including persistent binge eating cessation, reduction of obsessive-compulsive related binge eating symptoms, reduction of body-weight, and reduction of triglycerides.[45][50] Lisdexamfetamine, like all pharmaceutical amphetamines, has direct appetite suppressant effects that may be therapeutically useful in both BED and its comorbidities.[46][50] Based on reviews of neuroimaging studies involving BED-diagnosed participants, therapeautic neuroplasticity in dopaminergic and noradrenergic pathways from long-term use of lisdexamfetamine may be implicated in lasting improvements in the regulation of eating behaviors that are observed even after the drug is discontinued.[46][47][50]
Narcolepsy
editNarcolepsy is a chronic sleep-wake disorder that is associated with excessive daytime sleepiness, cataplexy, and sleep paralysis.[53] Patients with narcolepsy are diagnosed as either type 1 or type 2, with only the former presenting cataplexy symptoms.[54] Type 1 narcolepsy results from the loss of approximately 70,000 orexin-releasing neurons in the lateral hypothalamus, leading to significantly reduced cerebrospinal orexin levels;[55][56] this reduction is a diagnostic biomarker for type 1 narcolepsy.[54] Lateral hypothalamic orexin neurons innervate every component of the ascending reticular activating system (ARAS), which includes noradrenergic, dopaminergic, histaminergic, and serotonergic nuclei that promote wakefulness.[56][57]
Amphetamine’s therapeutic mode of action in narcolepsy primarily involves increasing monoamine neurotransmitter activity in the ARAS.[55][58][59] This includes noradrenergic neurons in the locus coeruleus, dopaminergic neurons in the ventral tegmental area, histaminergic neurons in the tuberomammillary nucleus, and serotonergic neurons in the dorsal raphe nucleus.[57][59] Dextroamphetamine, the more dopaminergic enantiomer of amphetamine, is particularly effective at promoting wakefulness because dopamine release has the greatest influence on cortical activation and cognitive arousal, relative to other monoamines.[55] In contrast, levoamphetamine may have a greater effect on cataplexy, a symptom more sensitive to the effects of norepinephrine and serotonin.[55] Noradrenergic and serotonergic nuclei in the ARAS are involved in the regulation of the REM sleep cycle and function as "REM-off" cells, with amphetamine's effect on norepinephrine and serotonin contributing to the suppression of REM sleep and a possible reduction of cataplexy at high doses.[55][54][57]
The American Academy of Sleep Medicine (AASM) 2021 clinical practice guideline conditionally recommends dextroamphetamine for the treatment of both type 1 and type 2 narcolepsy.[60] Treatment with pharmaceutical amphetamines is generally less preferred relative to other stimulants (e.g., modafinil) and is considered a third-line treatment option.[61][62][63] Medical reviews indicate that amphetamine is safe and effective for the treatment of narcolepsy.[55][61][60] Amphetamine appears to be most effective at improving symptoms associated with hypersomnolence, with three reviews finding clinically significant reductions in daytime sleepiness in patients with narcolepsy.[55][61][60] Additionally, these reviews suggest that amphetamine may dose-dependently improve cataplexy symptoms.[55][61][60] However, the quality of evidence for these findings is low and is consequently reflected in the AASM's conditional recommendation for dextroamphetamine as a treatment option for narcolepsy.[60]
Enhancing performance
editCognitive performance
editIn 2015, a systematic review and a meta-analysis of high quality clinical trials found that, when used at low (therapeutic) doses, amphetamine produces modest yet unambiguous improvements in cognition, including working memory, long-term episodic memory, inhibitory control, and some aspects of attention, in normal healthy adults;[64][65] these cognition-enhancing effects of amphetamine are known to be partially mediated through the indirect activation of both dopamine D1 receptor and α2-adrenergic receptor in the prefrontal cortex.[34][64] A systematic review from 2014 found that low doses of amphetamine also improve memory consolidation, in turn leading to improved recall of information.[66] Therapeutic doses of amphetamine also enhance cortical network efficiency, an effect which mediates improvements in working memory in all individuals.[34][67] Amphetamine and other ADHD stimulants also improve task saliency (motivation to perform a task) and increase arousal (wakefulness), in turn promoting goal-directed behavior.[34][68][69] Stimulants such as amphetamine can improve performance on difficult and boring tasks and are used by some students as a study and test-taking aid.[34][69][70] Based upon studies of self-reported illicit stimulant use, 5–35% of college students use diverted ADHD stimulants, which are primarily used for enhancement of academic performance rather than as recreational drugs.[71][72][73] However, high amphetamine doses that are above the therapeutic range can interfere with working memory and other aspects of cognitive control.[34][69]
Physical performance
editAmphetamine is used by some athletes for its psychological and athletic performance-enhancing effects, such as increased endurance and alertness;[74][75] however, non-medical amphetamine use is prohibited at sporting events that are regulated by collegiate, national, and international anti-doping agencies.[76][77] In healthy people at oral therapeutic doses, amphetamine has been shown to increase muscle strength, acceleration, athletic performance in anaerobic conditions, and endurance (i.e., it delays the onset of fatigue), while improving reaction time.[74][78][79] Amphetamine improves endurance and reaction time primarily through reuptake inhibition and release of dopamine in the central nervous system.[78][79][80] Amphetamine and other dopaminergic drugs also increase power output at fixed levels of perceived exertion by overriding a "safety switch", allowing the core temperature limit to increase in order to access a reserve capacity that is normally off-limits.[79][81][82] At therapeutic doses, the adverse effects of amphetamine do not impede athletic performance;[74][78] however, at much higher doses, amphetamine can induce effects that severely impair performance, such as rapid muscle breakdown and elevated body temperature.[83][78]
Available forms
editLisdexamfetamine is available as the dimesylate salt in the form of both oral capsules and chewable tablets.[7] A dose of 50 mg of lisdexamfetamine dimesylate is approximately equimolar to a 20 mg dose of dextroamphetamine sulfate or to 15 mg dextroamphetamine free-base in terms of the amount of dextroamphetamine contained.[13][84][85] Lisdexamfetamine capsules can be swallowed intact, or they can be opened and mixed into water, yogurt, or applesauce and consumed in that manner.[7][86]
Contraindications
editPharmaceutical lisdexamfetamine is contraindicated in people with hypersensitivity to amphetamine products or any of the formulation's inactive ingredients.[7] It is also contraindicated in patients who have used a monoamine oxidase inhibitor (MAOI) within the last 14 days.[7][87] Amphetamine products are contraindicated by the United States Food and Drug Administration (USFDA) in people with a history of drug abuse, heart disease, or severe agitation or anxiety, or in those currently experiencing arteriosclerosis, glaucoma, hyperthyroidism, or severe hypertension.[88] However, a European consensus statement on adult ADHD noted that stimulants do not worsen substance misuse in adults with ADHD and comorbid substance use disorder and should not be avoided in these individuals.[89] In any case, the statement noted that immediate-release stimulants should be avoided in those with both ADHD and substance use disorder and that slower-release stimulant formulations like OROS methylphenidate (Concerta) and lisdexamfetamine should be preferred due to their lower misuse potential.[89] Prescribing information approved by the Australian Therapeutic Goods Administration further contraindicates anorexia.[90]
Adverse effects
editProducts containing lisdexamfetamine have a comparable drug safety profile to those containing amphetamine.[19] The major side effects of lisdexamfetamine in short-term clinical trials (≥5% incidence) have included decreased appetite, insomnia, dry mouth, weight loss, irritability, upper abdominal pain, nausea, vomiting, diarrhea, constipation, increased heart rate, anxiety, dizziness, and feeling jittery.[7][15] Rates of side effects may vary in adults, adolescents, and children.[7] Rare but serious side effects of lisdexamfetamine may include mania, sudden cardiac death in those with underlying heart problems, stimulant psychosis, and serotonin syndrome.[15][7]
Interactions
edit- Acidifying agents: Drugs or foods that acidify the urine, such as ascorbic acid, increase urinary excretion of dextroamphetamine, thus decreasing the half-life and effectiveness of dextroamphetamine in the body.[7][88]
- Alkalinizing agents: Drugs or foods that alkalinize the urine, such as sodium bicarbonate, decrease urinary excretion of dextroamphetamine, thus increasing the half-life and effectiveness of dextroamphetamine in the body.[7][88]
- CYP2D6 inhibitors: Hydroxylation via the cytochrome P450 enzyme CYP2D6 is the major pathway of metabolism of dextroamphetamine.[91] Potent CYP2D6 inhibitors, such as paroxetine, fluoxetine, bupropion, and duloxetine, among others, may inhibit the metabolism of dextroamphetamine and thereby increase exposure to it.[91][7] Studies characterizing this potential interaction are currently lacking.[91] Concomitant use of lisdexamfetamine with CYP2D6 inhibitors may increase the risk of serotonin syndrome due to greater drug exposure.[7]
- Monoamine oxidase inhibitors: Concomitant use of MAOIs and central nervous system stimulants such as lisdexamfetamine can cause a hypertensive crisis.[7]
Pharmacology
editMechanism of action
editPharmacodynamics of amphetamine in a dopamine neuron
|
Lisdexamfetamine is an inactive prodrug that is converted in the body to dextroamphetamine, a pharmacologically active compound which is responsible for the drug's activity.[99] After oral ingestion, lisdexamfetamine is broken down by enzymes in red blood cells to form L-lysine, a naturally occurring essential amino acid, and dextroamphetamine.[7] The half-life of this conversion is roughly 1 hour. The conversion of lisdexamfetamine to dextroamphetamine is not affected by gastrointestinal pH and is unlikely to be affected by alterations in normal gastrointestinal transit times.[7][100] Studies show a linear relationship between peak plasma concentration of dextroamphetamine and lisdexamfetamine dose up to lisdexamfetamine doses of 250mg.[101]
The optical isomers of amphetamine, i.e., dextroamphetamine and levoamphetamine, are TAAR1 agonists and vesicular monoamine transporter 2 inhibitors that can enter monoamine neurons;[92][93] this allows them to release monoamine neurotransmitters (dopamine, norepinephrine, and serotonin, among others) from their storage sites in the presynaptic neuron, as well as prevent the reuptake of these neurotransmitters from the synaptic cleft.[92][93]
Lisdexamfetamine was developed with the goal of providing a long duration of effect that is consistent throughout the day, with reduced potential for abuse. The attachment of the amino acid lysine slows down the relative amount of dextroamphetamine available to the blood stream. Because no free dextroamphetamine is present in lisdexamfetamine capsules, dextroamphetamine does not become available through mechanical manipulation, such as crushing or simple extraction. A relatively sophisticated biochemical process is needed to produce dextroamphetamine from lisdexamfetamine.[100] As opposed to Adderall, which contains amphetamine salts in a 3:1 dextro:levo ratio, lisdexamfetamine is a single-enantiomer dextroamphetamine formula.[99][88] Studies conducted show that lisdexamfetamine dimesylate may have less abuse potential than dextroamphetamine and an abuse profile similar to diethylpropion at dosages that are FDA-approved for treatment of ADHD, but still has a high abuse potential when this dosage is exceeded by over 100%.[100]
Pharmacokinetics
editThe oral bioavailability of amphetamine varies with gastrointestinal pH;[83] it is well absorbed from the gut, and bioavailability is typically 90%.[103] Amphetamine is a weak base with a pKa of 9.9;[104] consequently, when the pH is basic, more of the drug is in its lipid soluble free base form, and more is absorbed through the lipid-rich cell membranes of the gut epithelium.[104][83] Conversely, an acidic pH means the drug is predominantly in a water-soluble cationic (salt) form, and less is absorbed.[104] Approximately 20% of amphetamine circulating in the bloodstream is bound to plasma proteins.[10] Following absorption, amphetamine readily distributes into most tissues in the body, with high concentrations occurring in cerebrospinal fluid and brain tissue.[105]
The half-lives of amphetamine enantiomers differ and vary with urine pH.[104] At normal urine pH, the half-lives of dextroamphetamine and levoamphetamine are 9–11 hours and 11–14 hours, respectively.[104] Highly acidic urine will reduce the enantiomer half-lives to 7 hours;[105] highly alkaline urine will increase the half-lives up to 34 hours.[105] The immediate-release and extended release variants of salts of both isomers reach peak plasma concentrations at 3 hours and 7 hours post-dose respectively.[104] Amphetamine is eliminated via the kidneys, with 30–40% of the drug being excreted unchanged at normal urinary pH.[104] When the urinary pH is basic, amphetamine is in its free base form, so less is excreted.[104] When urine pH is abnormal, the urinary recovery of amphetamine may range from a low of 1% to a high of 75%, depending mostly upon whether urine is too basic or acidic, respectively.[104] Following oral administration, amphetamine appears in urine within 3 hours.[105] Roughly 90% of ingested amphetamine is eliminated 3 days after the last oral dose.[105]
Lisdexamfetamine is a prodrug of dextroamphetamine.[13][106] It is not as sensitive to pH as amphetamine when being absorbed in the gastrointestinal tract.[106] Following absorption into the blood stream, lisdexamfetamine is completely converted by red blood cells to dextroamphetamine and the amino acid L-lysine by hydrolysis via undetermined aminopeptidase enzymes.[106][13][84] This is the rate-limiting step in the bioactivation of lisdexamfetamine.[13] The elimination half-life of lisdexamfetamine is generally less than 1 hour.[106][13] Due to the necessary conversion of lisdexamfetamine into dextroamphetamine, levels of dextroamphetamine with lisdexamfetamine peak about one hour later than with an equivalent dose of immediate-release dextroamphetamine.[13][84] Presumably due to its rate-limited activation by red blood cells, intravenous administration of lisdexamfetamine shows greatly delayed time to peak and reduced peak levels compared to intravenous administration of an equivalent dose of dextroamphetamine.[13] The pharmacokinetics of lisdexamfetamine are similar regardless of whether it is administered orally, intranasally, or intravenously.[13][84] Hence, in contrast to dextroamphetamine, parenteral use does not enhance the subjective effects of lisdexamfetamine.[13][84] Because of its behavior as a prodrug and its pharmacokinetic differences, lisdexamfetamine has a longer duration of therapeutic effect than immediate-release dextroamphetamine and shows reduced misuse potential.[13][84]
CYP2D6, dopamine β-hydroxylase (DBH), flavin-containing monooxygenase 3 (FMO3), butyrate-CoA ligase (XM-ligase), and glycine N-acyltransferase (GLYAT) are the enzymes known to metabolize amphetamine or its metabolites in humans.[sources 2] Amphetamine has a variety of excreted metabolic products, including 4-hydroxyamphetamine, 4-hydroxynorephedrine, 4-hydroxyphenylacetone, benzoic acid, hippuric acid, norephedrine, and phenylacetone.[104][107] Among these metabolites, the active sympathomimetics are 4-hydroxyamphetamine,[108] 4-hydroxynorephedrine,[109] and norephedrine.[110] The main metabolic pathways involve aromatic para-hydroxylation, aliphatic alpha- and beta-hydroxylation, N-oxidation, N-dealkylation, and deamination.[104][111] The known metabolic pathways, detectable metabolites, and metabolizing enzymes in humans include the following:
Metabolic pathways of amphetamine in humans[sources 2]
|
Chemistry
editLisdexamfetamine is a substituted amphetamine with an amide linkage formed by the condensation of dextroamphetamine with the carboxylate group of the essential amino acid L-lysine.[19] The reaction occurs with retention of stereochemistry, so the product lisdexamfetamine exists as a single stereoisomer. There are many possible names for lisdexamfetamine based on IUPAC nomenclature, but it is usually named as N-[(2S)-1-phenyl-2-propanyl]-L-lysinamide or (2S)-2,6-diamino-N-[(1S)-1-methyl-2-phenylethyl]hexanamide.[121] The condensation reaction occurs with loss of water:
- (S)-PhCH
2CH(CH
3)NH
2 + (S)-HOOCCH(NH
2)CH
2CH
2CH
2CH
2NH
2 → (S,S)-PhCH
2CH(CH
3)NHC(O)CH(NH
2)CH
2CH
2CH
2CH
2NH
2 + H
2O
Amine functional groups are vulnerable to oxidation in air and so pharmaceuticals containing them are usually formulated as salts where this moiety has been protonated. This increases stability, water solubility, and, by converting a molecular compound to an ionic compound, increases the melting point and thereby ensures a solid product.[122] In the case of lisdexamfetamine, this is achieved by reacting with two equivalents of methanesulfonic acid to produce the dimesylate salt, a water-soluble (792 mg mL−1) powder with a white to off-white color.[7]
- PhCH
2CH(CH
3)NHC(O)CH(NH
2)CH
2CH
2CH
2CH
2NH
2 + 2 CH
3SO
3H → [PhCH
2CH(CH
3)NHC(O)CH(NH+
3)CH
2CH
2CH
2CH
2NH+
3][CH
3SO−
3]
2
Comparison to other formulations
editLisdexamfetamine dimesylate is one marketed formulation delivering dextroamphetamine. The following table compares the drug to other amphetamine pharmaceuticals.
| drug | formula | molar mass [note 4] |
amphetamine base [note 5] |
amphetamine base in equal doses |
doses with equal base content [note 6] | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| (g/mol) | (percent) | (30 mg dose) | ||||||||
| total | base | total | dextro- | levo- | dextro- | levo- | ||||
| dextroamphetamine sulfate[124][125] | (C9H13N)2•H2SO4 | 368.49
|
270.41
|
73.38%
|
73.38%
|
—
|
22.0 mg
|
—
|
30.0 mg
| |
| amphetamine sulfate[126] | (C9H13N)2•H2SO4 | 368.49
|
270.41
|
73.38%
|
36.69%
|
36.69%
|
11.0 mg
|
11.0 mg
|
30.0 mg
| |
| Adderall | 62.57%
|
47.49%
|
15.08%
|
14.2 mg
|
4.5 mg
|
35.2 mg
| ||||
| 25% | dextroamphetamine sulfate[124][125] | (C9H13N)2•H2SO4 | 368.49
|
270.41
|
73.38%
|
73.38%
|
—
|
|||
| 25% | amphetamine sulfate[126] | (C9H13N)2•H2SO4 | 368.49
|
270.41
|
73.38%
|
36.69%
|
36.69%
|
|||
| 25% | dextroamphetamine saccharate[127] | (C9H13N)2•C6H10O8 | 480.55
|
270.41
|
56.27%
|
56.27%
|
—
|
|||
| 25% | amphetamine aspartate monohydrate[128] | (C9H13N)•C4H7NO4•H2O | 286.32
|
135.21
|
47.22%
|
23.61%
|
23.61%
|
|||
| lisdexamfetamine dimesylate[106] | C15H25N3O•(CH4O3S)2 | 455.49
|
135.21
|
29.68%
|
29.68%
|
—
|
8.9 mg
|
—
|
74.2 mg
| |
| amphetamine base suspension[129] | C9H13N | 135.21
|
135.21
|
100%
|
76.19%
|
23.81%
|
22.9 mg
|
7.1 mg
|
22.0 mg
| |
History
editLisdexamfetamine was developed by New River Pharmaceuticals, who were bought by Takeda Pharmaceuticals through its acquisition of Shire Pharmaceuticals, shortly before it began being marketed. It was developed with the intention of creating a longer-lasting and less-easily abused version of dextroamphetamine, as the requirement of conversion into dextroamphetamine via enzymes in the red blood cells delays its onset of action, regardless of the route of administration.[130]
In February 2007, the US Food and Drug Administration (FDA) approved lisdexamfetamine for the treatment of ADHD.[131] In August 2009, Health Canada approved the marketing of lisdexamfetamine for prescription use.[132]
In January 2015, lisdexamfetamine was approved by the FDA for treatment of binge eating disorder in adults.[133]
The FDA gave tentative approval to generic formulations of lisdexamfetamine in 2015.[134] The expiration date for patent protection of lisdexamfetamine in the US was 24 February 2023.[134] The Canadian patent expired 20 years from the filing date of 1 June 2004.[135]
Production quotas for 2016 in the United States were 29,750 kg.[136]
Society and culture
editName
editLisdexamfetamine is the International Nonproprietary Name (INN) and is a contraction of L-lysine-dextroamphetamine.[137]
As of November 2020, lisdexamfetamine is sold under the following brand names: Aduvanz, Elvanse, Juneve, Samexid, Tyvense, Venvanse, and Vyvanse.[138]
Research
editDepression
editAmphetamine was used to treat depression starting in the 1930s and has been described as the first antidepressant.[139] In clinical studies in the 1970s and 1980s, psychostimulants, including amphetamine and methylphenidate, were found to transiently improve mood in a majority of people with depression and to increase psychomotor activation in almost all individuals.[140]
Some clinical trials that used lisdexamfetamine as an add-on therapy with a selective serotonin reuptake inhibitor (SSRI) or serotonin-norepinephrine reuptake inhibitor (SNRI) for treatment-resistant depression indicated that this is no more effective than the use of an SSRI or SNRI alone.[141] Other studies indicated that psychostimulants potentiated antidepressants, and were under-prescribed for treatment resistant depression. In those studies, patients showed significant improvement in energy, mood, and psychomotor activity.[142] Clinical guidelines advise caution in the use of stimulants for depression and advise them only as second- or third-line adjunctive agents.[143]
In February 2014, Shire announced that two late-stage clinical trials had found that Vyvanse was not an effective treatment for depression, and development for this indication was discontinued.[144][145] A 2018 meta-analysis of randomized controlled trials of lisdexamfetamine for antidepressant augmentation in people with major depressive disorder—the first to be conducted—found that lisdexamfetamine was not significantly better than placebo in improving Montgomery–Åsberg Depression Rating Scale scores, response rates, or remission rates.[146] However, there was indication of a small effect in improving depressive symptoms that approached trend-level significance.[146] Lisdexamfetamine was well-tolerated in the meta-analysis.[146] The quantity of evidence was limited, with only four trials included.[146] In a subsequent 2022 network meta-analysis, lisdexamfetamine was significantly effective as an antidepressant augmentation for treatment-resistant depression.[143]
Although lisdexamfetamine has shown limited effectiveness in the treatment of depression in clinical trials, a phase II clinical study found that the addition of lisdexamfetamine to an antidepressant improved executive dysfunction in people with mild major depressive disorder but persisting executive dysfunction.[147][148]
Explanatory notes
edit- ^ The ADHD-related outcome domains with the greatest proportion of significantly improved outcomes from long-term continuous stimulant therapy include academics (≈55% of academic outcomes improved), driving (100% of driving outcomes improved), non-medical drug use (47% of addiction-related outcomes improved), obesity (≈65% of obesity-related outcomes improved), self-esteem (50% of self-esteem outcomes improved), and social function (67% of social function outcomes improved).[32]
The largest effect sizes for outcome improvements from long-term stimulant therapy occur in the domains involving academics (e.g., grade point average, achievement test scores, length of education, and education level), self-esteem (e.g., self-esteem questionnaire assessments, number of suicide attempts, and suicide rates), and social function (e.g., peer nomination scores, social skills, and quality of peer, family, and romantic relationships).[32]
Long-term combination therapy for ADHD (i.e., treatment with both a stimulant and behavioral therapy) produces even larger effect sizes for outcome improvements and improves a larger proportion of outcomes across each domain compared to long-term stimulant therapy alone.[32] - ^ Cochrane reviews are high quality meta-analytic systematic reviews of randomized controlled trials.[39]
- ^ 4-Hydroxyamphetamine has been shown to be metabolized into 4-hydroxynorephedrine by dopamine beta-hydroxylase (DBH) in vitro and it is presumed to be metabolized similarly in vivo.[112][116] Evidence from studies that measured the effect of serum DBH concentrations on 4-hydroxyamphetamine metabolism in humans suggests that a different enzyme may mediate the conversion of 4-hydroxyamphetamine to 4-hydroxynorephedrine;[116][118] however, other evidence from animal studies suggests that this reaction is catalyzed by DBH in synaptic vesicles within noradrenergic neurons in the brain.[119][120]
- ^ For uniformity, molar masses were calculated using the Lenntech Molecular Weight Calculator[123] and were within 0.01 g/mol of published pharmaceutical values.
- ^ Amphetamine base percentage = molecular massbase / molecular masstotal. Amphetamine base percentage for Adderall = sum of component percentages / 4.
- ^ dose = (1 / amphetamine base percentage) × scaling factor = (molecular masstotal / molecular massbase) × scaling factor. The values in this column were scaled to a 30 mg dose of dextroamphetamine sulfate. Due to pharmacological differences between these medications (e.g., differences in the release, absorption, conversion, concentration, differing effects of enantiomers, half-life, etc.), the listed values should not be considered equipotent doses.
Reference notes
editReferences
edit- ^ a b "Adderall vs Vyvanse - What's the difference between them?". Drugs.com. Retrieved 12 March 2022.
- ^ a b Goodman DW (May 2010). "Lisdexamfetamine dimesylate (vyvanse), a prodrug stimulant for attention-deficit/hyperactivity disorder". P & T. 35 (5): 273–287. PMC 2873712. PMID 20514273.
- ^ "FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)". nctr-crs.fda.gov. FDA. Retrieved 22 October 2023.
- ^ "Australian Product Information Vyanse® (Lisdexamfetamine dimesilate)" (PDF). Department of Health and Aged Care. Archived (PDF) from the original on 22 January 2023.
- ^ Anvisa (31 March 2023). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 4 April 2023). Archived from the original on 3 August 2023. Retrieved 3 August 2023.
- ^ "Vyvanse Product information". Health Canada. 15 December 2021. Retrieved 18 March 2024.
- ^ a b c d e f g h i j k l m n o p q r s t "Vyvanse- lisdexamfetamine dimesylate capsule; Vyvanse- lisdexamfetamine dimesylate tablet, chewable". DailyMed. 10 March 2022. Retrieved 19 December 2022.
- ^ "List of nationally authorised medicinal products : Active substance(s): lisdexamfetamine : Procedure No. PSUSA/00010289/202002" (PDF). Ema.europa.eu. Retrieved 12 March 2022.
- ^ "Public Assessment Report Decentralised Procedure" (PDF). MHRA. p. 14. Archived from the original (PDF) on 26 August 2014. Retrieved 23 August 2014.
- ^ a b Wishart DS, Djombou Feunang Y, Guo AC, Lo EJ, Marcu A, Grant JR, et al. "Amphetamine | DrugBank Online". DrugBank. 5.0.
- ^ a b Millichap JG (2010). "Chapter 9: Medications for ADHD". In Millichap JG (ed.). Attention Deficit Hyperactivity Disorder Handbook: A Physician's Guide to ADHD (2nd ed.). New York, USA: Springer. p. 112. ISBN 978-1-4419-1396-8.
Table 9.2 Dextroamphetamine formulations of stimulant medication
Dexedrine [Peak:2–3 h] [Duration:5–6 h] ...
Adderall [Peak:2–3 h] [Duration:5–7 h]
Dexedrine spansules [Peak:7–8 h] [Duration:12 h] ...
Adderall XR [Peak:7–8 h] [Duration:12 h]
Vyvanse [Peak:3–4 h] [Duration:12 h] - ^ a b Brams M, Mao AR, Doyle RL (September 2008). "Onset of efficacy of long-acting psychostimulants in pediatric attention-deficit/hyperactivity disorder". Postgraduate Medicine. 120 (3): 69–88. doi:10.3810/pgm.2008.09.1909. PMID 18824827. S2CID 31791162.
Onset of efficacy was earliest for d-MPH-ER at 0.5 hours, followed by d, l-MPH-LA at 1 to 2 hours, MCD at 1.5 hours, d, l-MPH-OR at 1 to 2 hours, MAS-XR at 1.5 to 2 hours, MTS at 2 hours, and LDX at approximately 2 hours. ... MAS-XR, and LDX have a long duration of action at 12 hours postdose
- ^ a b c d e f g h i j k l Ermer JC, Pennick M, Frick G (May 2016). "Lisdexamfetamine Dimesylate: Prodrug Delivery, Amphetamine Exposure and Duration of Efficacy". Clinical Drug Investigation. 36 (5): 341–356. doi:10.1007/s40261-015-0354-y. PMC 4823324. PMID 27021968.
- ^ a b Stahl SM (March 2017). "Lisdexamfetamine". Prescriber's Guide: Stahl's Essential Psychopharmacology (6th ed.). Cambridge, United Kingdom: Cambridge University Press. pp. 379–384. ISBN 978-1-108-22874-9.
- ^ a b c d e f g h i j k "Lisdexamfetamine Dimesylate Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists. Retrieved 15 April 2019.
- ^ a b British national formulary: BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 348–349. ISBN 978-0-85711-338-2.
- ^ "Lisdexamfetamine (Vyvanse) Use During Pregnancy". Drugs.com. Retrieved 16 April 2019.
- ^ Heal DJ, Smith SL, Gosden J, Nutt DJ (June 2013). "Amphetamine, past and present--a pharmacological and clinical perspective". Journal of Psychopharmacology. 27 (6): 479–496. doi:10.1177/0269881113482532. PMC 3666194. PMID 23539642.
- ^ a b c Blick SK, Keating GM (2007). "Lisdexamfetamine". Paediatric Drugs. 9 (2): 129–135, discussion 136–138. doi:10.2165/00148581-200709020-00007. PMID 17407369. S2CID 260863254.
- ^ "Shire's ADHD amphetamine wins British backing". Reuters. 12 December 2012. Retrieved 14 December 2023.
- ^ "The Top 300 of 2022". ClinCalc. Archived from the original on 30 August 2024. Retrieved 30 August 2024.
- ^ "Lisdexamfetamine Drug Usage Statistics, United States, 2013 - 2022". ClinCalc. Retrieved 30 August 2024.
- ^ Drugs of Abuse (PDF). Drug Enforcement Administration • U.S. Department of Justice. 2017. p. 22. Retrieved 16 April 2019.
- ^ Stuhec M, Lukić P, Locatelli I (February 2019). "Efficacy, Acceptability, and Tolerability of Lisdexamfetamine, Mixed Amphetamine Salts, Methylphenidate, and Modafinil in the Treatment of Attention-Deficit Hyperactivity Disorder in Adults: A Systematic Review and Meta-analysis". The Annals of Pharmacotherapy. 53 (2): 121–133. doi:10.1177/1060028018795703. PMID 30117329. S2CID 52019992.
- ^ Carvalho M, Carmo H, Costa VM, Capela JP, Pontes H, Remião F, et al. (August 2012). "Toxicity of amphetamines: an update". Archives of Toxicology. 86 (8): 1167–1231. Bibcode:2012ArTox..86.1167C. doi:10.1007/s00204-012-0815-5. PMID 22392347. S2CID 2873101.
- ^ Berman S, O'Neill J, Fears S, Bartzokis G, London ED (October 2008). "Abuse of amphetamines and structural abnormalities in the brain". Annals of the New York Academy of Sciences. 1141 (1): 195–220. doi:10.1196/annals.1441.031. PMC 2769923. PMID 18991959.
- ^ a b Hart H, Radua J, Nakao T, Mataix-Cols D, Rubia K (February 2013). "Meta-analysis of functional magnetic resonance imaging studies of inhibition and attention in attention-deficit/hyperactivity disorder: exploring task-specific, stimulant medication, and age effects". JAMA Psychiatry. 70 (2): 185–198. doi:10.1001/jamapsychiatry.2013.277. PMID 23247506.
- ^ a b Spencer TJ, Brown A, Seidman LJ, Valera EM, Makris N, Lomedico A, et al. (September 2013). "Effect of psychostimulants on brain structure and function in ADHD: a qualitative literature review of magnetic resonance imaging-based neuroimaging studies". The Journal of Clinical Psychiatry. 74 (9): 902–917. doi:10.4088/JCP.12r08287. PMC 3801446. PMID 24107764.
- ^ a b Frodl T, Skokauskas N (February 2012). "Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects". Acta Psychiatrica Scandinavica. 125 (2): 114–126. doi:10.1111/j.1600-0447.2011.01786.x. PMID 22118249. S2CID 25954331.
Basal ganglia regions like the right globus pallidus, the right putamen, and the nucleus caudatus are structurally affected in children with ADHD. These changes and alterations in limbic regions like ACC and amygdala are more pronounced in non-treated populations and seem to diminish over time from child to adulthood. Treatment seems to have positive effects on brain structure.
- ^ a b c d Huang YS, Tsai MH (July 2011). "Long-term outcomes with medications for attention-deficit hyperactivity disorder: current status of knowledge". CNS Drugs. 25 (7): 539–554. doi:10.2165/11589380-000000000-00000. PMID 21699268. S2CID 3449435.
Several other studies,[97-101] including a meta-analytic review[98] and a retrospective study,[97] suggested that stimulant therapy in childhood is associated with a reduced risk of subsequent substance use, cigarette smoking and alcohol use disorders. ... Recent studies have demonstrated that stimulants, along with the non-stimulants atomoxetine and extended-release guanfacine, are continuously effective for more than 2-year treatment periods with few and tolerable adverse effects. The effectiveness of long-term therapy includes not only the core symptoms of ADHD, but also improved quality of life and academic achievements. The most concerning short-term adverse effects of stimulants, such as elevated blood pressure and heart rate, waned in long-term follow-up studies. ... The current data do not support the potential impact of stimulants on the worsening or development of tics or substance abuse into adulthood. In the longest follow-up study (of more than 10 years), lifetime stimulant treatment for ADHD was effective and protective against the development of adverse psychiatric disorders.
- ^ a b c Millichap JG (2010). "Chapter 9: Medications for ADHD". In Millichap JG (ed.). Attention Deficit Hyperactivity Disorder Handbook: A Physician's Guide to ADHD (2nd ed.). New York, US: Springer. pp. 121–123, 125–127. ISBN 9781441913968.
Ongoing research has provided answers to many of the parents' concerns, and has confirmed the effectiveness and safety of the long-term use of medication.
- ^ a b c d e Arnold LE, Hodgkins P, Caci H, Kahle J, Young S (February 2015). "Effect of treatment modality on long-term outcomes in attention-deficit/hyperactivity disorder: a systematic review". PLOS ONE. 10 (2): e0116407. doi:10.1371/journal.pone.0116407. PMC 4340791. PMID 25714373.
The highest proportion of improved outcomes was reported with combination treatment (83% of outcomes). Among significantly improved outcomes, the largest effect sizes were found for combination treatment. The greatest improvements were associated with academic, self-esteem, or social function outcomes.
Figure 3: Treatment benefit by treatment type and outcome group - ^ a b c Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 6: Widely Projecting Systems: Monoamines, Acetylcholine, and Orexin". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York, US: McGraw-Hill Medical. pp. 154–157. ISBN 9780071481274.
- ^ a b c d e f Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 13: Higher Cognitive Function and Behavioral Control". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York, US: McGraw-Hill Medical. pp. 318, 321. ISBN 9780071481274.
Therapeutic (relatively low) doses of psychostimulants, such as methylphenidate and amphetamine, improve performance on working memory tasks both in normal subjects and those with ADHD. ... stimulants act not only on working memory function, but also on general levels of arousal and, within the nucleus accumbens, improve the saliency of tasks. Thus, stimulants improve performance on effortful but tedious tasks ... through indirect stimulation of dopamine and norepinephrine receptors. ...
Beyond these general permissive effects, dopamine (acting via D1 receptors) and norepinephrine (acting at several receptors) can, at optimal levels, enhance working memory and aspects of attention. - ^ Bidwell LC, McClernon FJ, Kollins SH (August 2011). "Cognitive enhancers for the treatment of ADHD". Pharmacology Biochemistry and Behavior. 99 (2): 262–274. doi:10.1016/j.pbb.2011.05.002. PMC 3353150. PMID 21596055.
- ^ Parker J, Wales G, Chalhoub N, Harpin V (September 2013). "The long-term outcomes of interventions for the management of attention-deficit hyperactivity disorder in children and adolescents: a systematic review of randomized controlled trials". Psychology Research and Behavior Management. 6: 87–99. doi:10.2147/PRBM.S49114. PMC 3785407. PMID 24082796.
Only one paper53 examining outcomes beyond 36 months met the review criteria. ... There is high level evidence suggesting that pharmacological treatment can have a major beneficial effect on the core symptoms of ADHD (hyperactivity, inattention, and impulsivity) in approximately 80% of cases compared with placebo controls, in the short term.
- ^ Millichap JG (2010). "Chapter 9: Medications for ADHD". In Millichap JG (ed.). Attention Deficit Hyperactivity Disorder Handbook: A Physician's Guide to ADHD (2nd ed.). New York, US: Springer. pp. 111–113. ISBN 9781441913968.
- ^ "Stimulants for Attention Deficit Hyperactivity Disorder". WebMD. Healthwise. 12 April 2010. Retrieved 12 November 2013.
- ^ Scholten RJ, Clarke M, Hetherington J (August 2005). "The Cochrane Collaboration". European Journal of Clinical Nutrition. 59 (Suppl 1): S147–S149, discussion S195–S196. doi:10.1038/sj.ejcn.1602188. PMID 16052183. S2CID 29410060.
- ^ Castells X, Blanco-Silvente L, Cunill R (August 2018). "Amphetamines for attention deficit hyperactivity disorder (ADHD) in adults". Cochrane Database of Systematic Reviews. 2018 (8): CD007813. doi:10.1002/14651858.CD007813.pub3. PMC 6513464. PMID 30091808.
- ^ Punja S, Shamseer L, Hartling L, Urichuk L, Vandermeer B, Nikles J, et al. (February 2016). "Amphetamines for attention deficit hyperactivity disorder (ADHD) in children and adolescents". Cochrane Database of Systematic Reviews. 2016 (2): CD009996. doi:10.1002/14651858.CD009996.pub2. PMC 10329868. PMID 26844979.
- ^ Osland ST, Steeves TD, Pringsheim T (June 2018). "Pharmacological treatment for attention deficit hyperactivity disorder (ADHD) in children with comorbid tic disorders". Cochrane Database of Systematic Reviews. 2018 (6): CD007990. doi:10.1002/14651858.CD007990.pub3. PMC 6513283. PMID 29944175.
- ^ a b Giel KE, Bulik CM, Fernandez-Aranda F, Hay P, Keski-Rahkonen A, Schag K, et al. (March 2022). "Binge eating disorder". Nature Reviews. Disease Primers. 8 (1): 16. doi:10.1038/s41572-022-00344-y. PMC 9793802. PMID 35301358.
- ^ a b c d Heal DJ, Smith SL (June 2022). "Prospects for new drugs to treat binge-eating disorder: Insights from psychopathology and neuropharmacology". Journal of Psychopharmacology. 36 (6): 680–703. doi:10.1177/02698811211032475. PMC 9150143. PMID 34318734.
BED subjects have substantial decrements in their ventral striatal reward pathways and diminished ability to recruit fronto-cortical impulse-control circuits to implement dietary restraint. ...
There is not only substantial overlap between the psychopathology of BED and ADHD but also a clear association between these two disorders. Lisdexamfetamine's ability to reduce impulsivity and increase cognitive control in ADHD supports the hypothesis that efficacy in BED is dependent on treating its core obsessive, compulsive and impulsive behaviours. - ^ a b c d e McElroy SL (2017). "Pharmacologic Treatments for Binge-Eating Disorder". The Journal of Clinical Psychiatry. 78 Suppl 1: 14–19. doi:10.4088/JCP.sh16003su1c.03. PMID 28125174.
Genetic polymorphisms associated with abnormal dopaminergic signaling have been found in individuals who exhibit binge-eating behavior, and the binge-eating episodes,which often involve the consumption of highly palatable food, further stimulate the dopaminergic system. This ongoing stimulation may contribute to progressive impairments in dopamine signaling. Lisdexamfetamine is hypothesized to reduce binge-eating behavior by normalizing dopaminergic activity. ...
After 12 weeks, both studies found significant reductions in the number of binge-eating days per week in the active treatment group compared with placebo (P < .001 for both studies; Figure 1). Lisdexamfetamine was also found to be superior to placebo on a number of secondary outcome measures including global improvement, binge-eating cessation for 4 weeks, and reduction of obsessive-compulsive binge-eating symptoms, body weight, and triglycerides. - ^ a b c d Rodan SC, Bryant E, Le A, Maloney D, Touyz S, McGregor IS, et al. (July 2023). "Pharmacotherapy, alternative and adjunctive therapies for eating disorders: findings from a rapid review". Journal of Eating Disorders. 11 (1): 112. doi:10.1186/s40337-023-00833-9. PMC 10327007. PMID 37415200.
LDX is commonly used in the treatment of ADHD, and is the only treatment for BED that is currently approved by the Food and Drug Administration (FDA) and the Therapeutic Goods Administration (TGA). LDX, like all amphetamine stimulants, has direct appetite suppressant effects that may be therapeutically useful in BED, although long-term neuroadaptations in dopaminergic and noradrenergic systems caused by LDX may also be relevant, leading to improved regulation of eating behaviours, attentional processes and goal-directed behaviours. ...
Evidently, there is a substantial volume of trials with high-quality evidence supporting the efficacy of LDX in reducing binge eating frequency in treatment of adults with moderate to severe BED at 50–70 mg/day. - ^ a b c d e Boswell RG, Potenza MN, Grilo CM (January 2021). "The Neurobiology of Binge-eating Disorder Compared with Obesity: Implications for Differential Therapeutics". Clinical Therapeutics. 43 (1): 50–69. doi:10.1016/j.clinthera.2020.10.014. PMC 7902428. PMID 33257092.
Stimulant medications may be especially effective for individuals with BED because of dual effects on reward and executive function systems. Indeed, the only FDA-approved pharmacotherapy for BED is LDX, a d-amphetamine prodrug. ...
In humans, RCTs found that LDX reduced binge eating and impulsivity/compulsivity symptoms. Notably, there is a strong correlation between compulsivity symptoms and severity/frequency of binge eating episodes observed in LDX trials. Further, in individuals with BED, changes in prefrontal brain systems associated with LDX treatment were related to treatment outcome. - ^ a b c d Berry MD, Gainetdinov RR, Hoener MC, Shahid M (December 2017). "Pharmacology of human trace amine-associated receptors: Therapeutic opportunities and challenges". Pharmacology & Therapeutics. 180: 161–180. doi:10.1016/j.pharmthera.2017.07.002. PMID 28723415.
- ^ Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 14: Higher Cognitive Function and Behavioral Control". Molecular neuropharmacology: a foundation for clinical neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 9780071827706.
Because behavioral responses in humans are not rigidly dictated by sensory inputs and drives, behavioral responses can instead be guided in accordance with short- or long-term goals, prior experience, and the environmental context. The response to a delicious-looking dessert is different depending on whether a person is alone staring into his or her refrigerator, is at a formal dinner party attended by his or her punctilious boss, or has just formulated the goal of losing 10 lb. ...
Adaptive responses depend on the ability to inhibit automatic or prepotent responses (eg, to ravenously eat the dessert or run from the snake) given certain social or environmental contexts or chosen goals and, in those circumstances, to select more appropriate responses. In conditions in which prepotent responses tend to dominate behavior, such as in drug addiction, where drug cues can elicit drug seeking (Chapter 16), or inattention deficit hyperactivity disorder (ADHD; described below), significant negative consequences can result. - ^ a b c d e f g Schneider E, Higgs S, Dourish CT (December 2021). "Lisdexamfetamine and binge-eating disorder: A systematic review and meta-analysis of the preclinical and clinical data with a focus on mechanism of drug action in treating the disorder" (PDF). European Neuropsychopharmacology. 53: 49–78. doi:10.1016/j.euroneuro.2021.08.001. PMID 34461386.
Our meta-analysis of the four RCT data sets (Guerdjikova et al., 2016; McElroy et al., 2015b; McElroy et al., 2016a) showed an overall significant effect of LDX on binge-eating symptom change. ...
BED has been described as an impulse control disorder since one of the key symptoms of the disorder is a lack of control over eating (American Psychiatric Association, 2013) and it is possible that LDX may be effective in treating BED at least in part by reducing impulsivity, compulsivity, and the repetitive nature of binge eating. There is extensive evidence that loss of impulse control in BED is a causal factor in provoking bingeing symptoms (Colles et al., 2008; Galanti et al., 2007; Giel et al., 2017; McElroy et al., 2016a; Nasser et al., 2004; Schag et al., 2013). More specifically, BED is associated with motor impulsivity and non-planning impulsivity which could initiate and maintain binge eating (Nasser et al., 2004). Neuroimaging studies using the Stroop task to measure impulse control have shown that BED patients have decreased BOLD fMRI activity in brain areas involved in self-regulation and impulse control including VMPFC, inferior frontal gyrus (IFG), and insula during performance of the task compared to lean and obese controls (Balodis et al., 2013b). ...
It is conceivable that in BED patients a low 30 mg dose of LDX could reduce food intake by suppressing appetite or enhancing satiety and higher (50 and 70 mg) doses of the drug may have a dual suppressant effect on food intake and binge-eating frequency. - ^ Branis NM, Wittlin SD (2015). "Amphetamine-Like Analogues in Diabetes: Speeding towards Ketogenesis". Case Reports in Endocrinology. 2015: 917869. doi:10.1155/2015/917869. PMC 4417573. PMID 25960894.
Peripheral norepinephrine concentration rises as well. As demonstrated after Dextroamphetamine administration, plasma norepinephrine can rise up to 400 pg/mL, a level comparable to that achieved during mild physical activity. Cumulative effect on norepinephrine concentration is likely when amphetamine-type medications are given in the setting of acute illness or combined with activities leading to catecholamine release, such as exercise. ... The primary effect of norepinephrine on ketogenesis is mediated through increased substrate availability. As shown by Krentz et al., at high physiological concentrations, norepinephrine induces accelerated lipolysis and increases NEFA formation significantly. Secondly, norepinephrine stimulates ketogenesis directly at the hepatocyte level. As reported by Keller et al., norepinephrine infusion increased ketone bodies concentration to a greater degree when compared to NEFA concentration (155 ± 30 versus 57 ± 16%), suggesting direct hepatic ketogenic effect.
- ^ Muratore AF, Attia E (July 2022). "Psychopharmacologic Management of Eating Disorders". Current Psychiatry Reports. 24 (7): 345–351. doi:10.1007/s11920-022-01340-5. PMC 9233107. PMID 35576089.
An 11-week, double-blind RCT examined the effects of three doses of lisdexamfetamine (30 mg/day, 50 mg/day, 70 mg/day) and placebo on binge eating frequency. Results indicated that 50 mg and 70 mg doses were superior to placebo in reducing binge eating. Two follow-up 12-week RCTs confirmed the superiority of 50 and 70 mg doses to placebo in improving binge eating and secondary outcome measures, including obsessive–compulsive symptoms, body weight, and global improvement. ... Subsequent studies of lisdexamfetamine provided further support for the medication's safety and efficacy and provided additional evidence that continued use may be better than placebo in preventing relapse. While it is considered safe and effective, lisdexamfetamine's side effect profile and risk for misuse may make it inappropriate for certain patients.
- ^ Mahlios J, De la Herrán-Arita AK, Mignot E (October 2013). "The autoimmune basis of narcolepsy". Current Opinion in Neurobiology. 23 (5): 767–773. doi:10.1016/j.conb.2013.04.013. PMC 3848424. PMID 23725858.
- ^ a b c Barateau L, Pizza F, Plazzi G, Dauvilliers Y (August 2022). "Narcolepsy". Journal of Sleep Research. 31 (4): e13631. doi:10.1111/jsr.13631. PMID 35624073.
Narcolepsy type 1 was called "narcolepsy with cataplexy" before 2014 (AASM, 2005), but was renamed NT1 in the third and last international classification of sleep disorders (AASM, 2014). ... A low level of Hcrt-1 in the CSF is very sensitive and specific for the diagnosis of NT1. ...
All patients with low CSF Hcrt-1 levels are considered as NT1 patients, even if they report no cataplexy (in about 10–20% of cases), and all patients with normal CSF Hcrt-1 levels (or without cataplexy when the lumbar puncture is not performed) as NT2 patients (Baumann et al., 2014). ...
In patients with NT1, the absence of Hcrt leads to the inhibition of regions that suppress REM sleep, thus allowing the activation of descending pathways inhibiting motoneurons, leading to cataplexy. - ^ a b c d e f g h Mignot EJ (October 2012). "A practical guide to the therapy of narcolepsy and hypersomnia syndromes". Neurotherapeutics. 9 (4): 739–752. doi:10.1007/s13311-012-0150-9. PMC 3480574. PMID 23065655.
At the pathophysiological level, it is now clear that most narcolepsy cases with cataplexy, and a minority of cases (5–30 %) without cataplexy or with atypical cataplexy-like symptoms, are caused by a lack of hypocretin (orexin) of likely an autoimmune origin. In these cases, once the disease is established, the majority of the 70,000 hypocretin-producing cells have been destroyed, and the disorder is irreversible. ...
Amphetamines are exceptionally wake-promoting, and at high doses also reduce cataplexy in narcoleptic patients, an effect best explained by its action on adrenergic and serotoninergic synapses. ...
The D-isomer is more specific for DA transmission and is a better stimulant compound. Some effects on cataplexy (especially for the L-isomer), secondary to adrenergic effects, occur at higher doses. ...
Numerous studies have shown that increased dopamine release is the main property explaining wake-promotion, although norepinephrine effects also contribute. - ^ a b Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 10: Neural and Neuroendocrine Control of the Internal Milieu". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. pp. 456–457. ISBN 9780071827706.
More recently, the lateral hypothalamus was also found to play a central role in arousal. Neurons in this region contain cell bodies that produce the orexin (also called hypocretin) peptides (Chapter 6). These neurons project widely throughout the brain and are involved in sleep, arousal, feeding, reward,aspects of emotion, and learning. In fact, orexin is thought to promote feeding primarily by promoting arousal. Mutations in orexin receptors are responsible for narcolepsy in a canine model, knockout of the orexin gene produces narcolepsy in mice, and humans with narcolepsy have low or absent levels of orexin peptides in cerebrospinal fluid (Chapter 13). Lateral hypothalamus neurons have reciprocal connections with neurons that produce monoamine neurotransmitters (Chapter 6).
- ^ a b c Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 13: Sleep and Arousal". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). McGraw-Hill Medical. p. 521. ISBN 9780071827706.
The ARAS consists of several different circuits including the four main monoaminergic pathways discussed in Chapter 6. The norepinephrine pathway originates from the LC and related brainstem nuclei; the serotonergic neurons originate from the RN within the brainstem as well; the dopaminergic neurons originate in the ventral tegmental area (VTA); and the histaminergic pathway originates from neurons in the tuberomammillary nucleus (TMN) of the posterior hypothalamus. As discussed in Chapter 6, these neurons project widely throughout the brain from restricted collections of cell bodies. Norepinephrine, serotonin,dopamine, and histamine have complex modulatory functions and, in general, promote wakefulness. The PT in the brainstem is also an important component of the ARAS. Activity of PT cholinergic neurons (REM-on cells) promotes REM sleep, as noted earlier. During waking, REM-on cells are inhibited by a subset of ARAS norepinephrine and serotonin neurons called REM-off cells.
- ^ Shneerson JM (2009). Sleep medicine a guide to sleep and its disorders (2nd ed.). John Wiley & Sons. p. 81. ISBN 9781405178518.
All the amphetamines enhance activity at dopamine, noradrenaline and 5HT synapses. They cause presynaptic release of preformed transmitters, and also inhibit the re-uptake of dopamine and noradrenaline. These actions are most prominent in the brainstem ascending reticular activating system and the cerebral cortex.
- ^ a b Schwartz JR, Roth T (2008). "Neurophysiology of sleep and wakefulness: basic science and clinical implications". Current Neuropharmacology. 6 (4): 367–378. doi:10.2174/157015908787386050. PMC 2701283. PMID 19587857.
Alertness and associated forebrain and cortical arousal are mediated by several ascending pathways with distinct neuronal components that project from the upper brain stem near the junction of the pons and the midbrain. ...
Key cell populations of the ascending arousal pathway include cholinergic, noradrenergic, serotoninergic, dopaminergic, and histaminergic neurons located in the pedunculopontine and laterodorsal tegmental nucleus (PPT/LDT), locus coeruleus, dorsal and median raphe nucleus, and tuberomammillary nucleus (TMN), respectively. ...
The mechanism of action of sympathomimetic alerting drugs (eg, dextro- and methamphetamine, methylphenidate) is direct or indirect stimulation of dopaminergic and noradrenergic nuclei, which in turn heightens the efficacy of the ventral periaqueductal grey area and locus coeruleus, both components of the secondary branch of the ascending arousal system. ...
Sympathomimetic drugs have long been used to treat narcolepsy - ^ a b c d e Maski K, Trotti LM, Kotagal S, Robert Auger R, Rowley JA, Hashmi SD, et al. (September 2021). "Treatment of central disorders of hypersomnolence: an American Academy of Sleep Medicine clinical practice guideline". Journal of Clinical Sleep Medicine. 17 (9): 1881–1893. doi:10.5664/jcsm.9328. PMC 8636351. PMID 34743789.
The TF identified 1 double-blind RCT, 1 single-blind RCT, and 1 retrospective observational long-term self-reported case series assessing the efficacy of dextroamphetamine in patients with narcolepsy type 1 and narcolepsy type 2. These studies demonstrated clinically significant improvements in excessive daytime sleepiness and cataplexy.
- ^ a b c d Barateau L, Lopez R, Dauvilliers Y (October 2016). "Management of Narcolepsy". Current Treatment Options in Neurology. 18 (10): 43. doi:10.1007/s11940-016-0429-y. PMID 27549768.
The usefulness of amphetamines is limited by a potential risk of abuse, and their cardiovascular adverse effects (Table 1). That is why, even though they are cheaper than other drugs, and efficient, they remain third-line therapy in narcolepsy. Three class II studies showed an improvement of EDS in that disease. ...
Despite the potential for drug abuse or tolerance using stimulants, patients with narcolepsy rarely exhibit addiction to their medication. ...
Some stimulants, such as mazindol, amphetamines, and pitolisant, may also have some anticataplectic effects. - ^ Dauvilliers Y, Barateau L (August 2017). "Narcolepsy and Other Central Hypersomnias". Continuum. 23 (4, Sleep Neurology): 989–1004. doi:10.1212/CON.0000000000000492. PMID 28777172.
Recent clinical trials and practice guidelines have confirmed that stimulants such as modafinil, armodafinil, or sodium oxybate (as first line); methylphenidate and pitolisant (as second line [pitolisant is currently only available in Europe]); and amphetamines (as third line) are appropriate medications for excessive daytime sleepiness.
- ^ Thorpy MJ, Bogan RK (April 2020). "Update on the pharmacologic management of narcolepsy: mechanisms of action and clinical implications". Sleep Medicine. 68: 97–109. doi:10.1016/j.sleep.2019.09.001. PMID 32032921.
The first agents used to treat EDS (ie, amphetamines, methylphenidate) are now considered second- or third-line options because newer medications have been developed with improved tolerability and lower abuse potential (eg, modafinil/armodafinil, solriamfetol, pitolisant)
- ^ a b Spencer RC, Devilbiss DM, Berridge CW (June 2015). "The Cognition-Enhancing Effects of Psychostimulants Involve Direct Action in the Prefrontal Cortex". Biological Psychiatry. 77 (11): 940–950. doi:10.1016/j.biopsych.2014.09.013. PMC 4377121. PMID 25499957.
The procognitive actions of psychostimulants are only associated with low doses. Surprisingly, despite nearly 80 years of clinical use, the neurobiology of the procognitive actions of psychostimulants has only recently been systematically investigated. Findings from this research unambiguously demonstrate that the cognition-enhancing effects of psychostimulants involve the preferential elevation of catecholamines in the PFC and the subsequent activation of norepinephrine α2 and dopamine D1 receptors. ... This differential modulation of PFC-dependent processes across dose appears to be associated with the differential involvement of noradrenergic α2 versus α1 receptors. Collectively, this evidence indicates that at low, clinically relevant doses, psychostimulants are devoid of the behavioral and neurochemical actions that define this class of drugs and instead act largely as cognitive enhancers (improving PFC-dependent function). ... In particular, in both animals and humans, lower doses maximally improve performance in tests of working memory and response inhibition, whereas maximal suppression of overt behavior and facilitation of attentional processes occurs at higher doses.
- ^ Ilieva IP, Hook CJ, Farah MJ (June 2015). "Prescription Stimulants' Effects on Healthy Inhibitory Control, Working Memory, and Episodic Memory: A Meta-analysis". Journal of Cognitive Neuroscience. 27 (6): 1069–1089. doi:10.1162/jocn_a_00776. PMID 25591060. S2CID 15788121.
Specifically, in a set of experiments limited to high-quality designs, we found significant enhancement of several cognitive abilities. ... The results of this meta-analysis ... do confirm the reality of cognitive enhancing effects for normal healthy adults in general, while also indicating that these effects are modest in size.
- ^ Bagot KS, Kaminer Y (April 2014). "Efficacy of stimulants for cognitive enhancement in non-attention deficit hyperactivity disorder youth: a systematic review". Addiction. 109 (4): 547–557. doi:10.1111/add.12460. PMC 4471173. PMID 24749160.
Amphetamine has been shown to improve consolidation of information (0.02 ≥ P ≤ 0.05), leading to improved recall.
- ^ Devous MD, Trivedi MH, Rush AJ (April 2001). "Regional cerebral blood flow response to oral amphetamine challenge in healthy volunteers". Journal of Nuclear Medicine. 42 (4): 535–542. PMID 11337538.
- ^ Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 10: Neural and Neuroendocrine Control of the Internal Milieu". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York, US: McGraw-Hill Medical. p. 266. ISBN 9780071481274.
Dopamine acts in the nucleus accumbens to attach motivational significance to stimuli associated with reward.
- ^ a b c Wood S, Sage JR, Shuman T, Anagnostaras SG (January 2014). "Psychostimulants and cognition: a continuum of behavioral and cognitive activation". Pharmacological Reviews. 66 (1): 193–221. doi:10.1124/pr.112.007054. PMC 3880463. PMID 24344115.
- ^ Twohey M (26 March 2006). "Pills become an addictive study aid". JS Online. Archived from the original on 15 August 2007. Retrieved 2 December 2007.
- ^ Teter CJ, McCabe SE, LaGrange K, Cranford JA, Boyd CJ (October 2006). "Illicit use of specific prescription stimulants among college students: prevalence, motives, and routes of administration". Pharmacotherapy. 26 (10): 1501–1510. doi:10.1592/phco.26.10.1501. PMC 1794223. PMID 16999660.
- ^ Weyandt LL, Oster DR, Marraccini ME, Gudmundsdottir BG, Munro BA, Zavras BM, et al. (September 2014). "Pharmacological interventions for adolescents and adults with ADHD: stimulant and nonstimulant medications and misuse of prescription stimulants". Psychology Research and Behavior Management. 7: 223–249. doi:10.2147/PRBM.S47013. PMC 4164338. PMID 25228824.
misuse of prescription stimulants has become a serious problem on college campuses across the US and has been recently documented in other countries as well. ... Indeed, large numbers of students claim to have engaged in the nonmedical use of prescription stimulants, which is reflected in lifetime prevalence rates of prescription stimulant misuse ranging from 5% to nearly 34% of students.
- ^ Clemow DB, Walker DJ (September 2014). "The potential for misuse and abuse of medications in ADHD: a review". Postgraduate Medicine. 126 (5): 64–81. doi:10.3810/pgm.2014.09.2801. PMID 25295651. S2CID 207580823.
Overall, the data suggest that ADHD medication misuse and diversion are common health care problems for stimulant medications, with the prevalence believed to be approximately 5% to 10% of high school students and 5% to 35% of college students, depending on the study.
- ^ a b c Liddle DG, Connor DJ (June 2013). "Nutritional supplements and ergogenic AIDS". Primary Care: Clinics in Office Practice. 40 (2): 487–505. doi:10.1016/j.pop.2013.02.009. PMID 23668655.
Amphetamines and caffeine are stimulants that increase alertness, improve focus, decrease reaction time, and delay fatigue, allowing for an increased intensity and duration of training ...
Physiologic and performance effects
• Amphetamines increase dopamine/norepinephrine release and inhibit their reuptake, leading to central nervous system (CNS) stimulation
• Amphetamines seem to enhance athletic performance in anaerobic conditions 39 40
• Improved reaction time
• Increased muscle strength and delayed muscle fatigue
• Increased acceleration
• Increased alertness and attention to task - ^ Westfall DP, Westfall TC (2010). "Miscellaneous Sympathomimetic Agonists". In Brunton LL, Chabner BA, Knollmann BC (eds.). Goodman & Gilman's Pharmacological Basis of Therapeutics (12th ed.). New York, US: McGraw-Hill. ISBN 9780071624428.
- ^ Bracken NM (January 2012). "National Study of Substance Use Trends Among NCAA College Student-Athletes" (PDF). NCAA Publications. National Collegiate Athletic Association. Archived (PDF) from the original on 9 October 2022. Retrieved 8 October 2013.
- ^ Docherty JR (June 2008). "Pharmacology of stimulants prohibited by the World Anti-Doping Agency (WADA)". British Journal of Pharmacology. 154 (3): 606–622. doi:10.1038/bjp.2008.124. PMC 2439527. PMID 18500382.
- ^ a b c d Parr JW (July 2011). "Attention-deficit hyperactivity disorder and the athlete: new advances and understanding". Clinics in Sports Medicine. 30 (3): 591–610. doi:10.1016/j.csm.2011.03.007. PMID 21658550.
In 1980, Chandler and Blair47 showed significant increases in knee extension strength, acceleration, anaerobic capacity, time to exhaustion during exercise, pre-exercise and maximum heart rates, and time to exhaustion during maximal oxygen consumption (VO2 max) testing after administration of 15 mg of dextroamphetamine versus placebo. Most of the information to answer this question has been obtained in the past decade through studies of fatigue rather than an attempt to systematically investigate the effect of ADHD drugs on exercise.
- ^ a b c Roelands B, de Koning J, Foster C, Hettinga F, Meeusen R (May 2013). "Neurophysiological determinants of theoretical concepts and mechanisms involved in pacing". Sports Medicine. 43 (5): 301–311. doi:10.1007/s40279-013-0030-4. PMID 23456493. S2CID 30392999.
In high-ambient temperatures, dopaminergic manipulations clearly improve performance. The distribution of the power output reveals that after dopamine reuptake inhibition, subjects are able to maintain a higher power output compared with placebo. ... Dopaminergic drugs appear to override a safety switch and allow athletes to use a reserve capacity that is 'off-limits' in a normal (placebo) situation.
- ^ Parker KL, Lamichhane D, Caetano MS, Narayanan NS (October 2013). "Executive dysfunction in Parkinson's disease and timing deficits". Frontiers in Integrative Neuroscience. 7: 75. doi:10.3389/fnint.2013.00075. PMC 3813949. PMID 24198770.
Manipulations of dopaminergic signaling profoundly influence interval timing, leading to the hypothesis that dopamine influences internal pacemaker, or "clock," activity. For instance, amphetamine, which increases concentrations of dopamine at the synaptic cleft advances the start of responding during interval timing, whereas antagonists of D2 type dopamine receptors typically slow timing;... Depletion of dopamine in healthy volunteers impairs timing, while amphetamine releases synaptic dopamine and speeds up timing.
- ^ Rattray B, Argus C, Martin K, Northey J, Driller M (March 2015). "Is it time to turn our attention toward central mechanisms for post-exertional recovery strategies and performance?". Frontiers in Physiology. 6: 79. doi:10.3389/fphys.2015.00079. PMC 4362407. PMID 25852568.
Aside from accounting for the reduced performance of mentally fatigued participants, this model rationalizes the reduced RPE and hence improved cycling time trial performance of athletes using a glucose mouthwash (Chambers et al., 2009) and the greater power output during a RPE matched cycling time trial following amphetamine ingestion (Swart, 2009). ... Dopamine stimulating drugs are known to enhance aspects of exercise performance (Roelands et al., 2008)
- ^ Roelands B, De Pauw K, Meeusen R (June 2015). "Neurophysiological effects of exercise in the heat". Scandinavian Journal of Medicine & Science in Sports. 25 (Suppl 1): 65–78. doi:10.1111/sms.12350. PMID 25943657. S2CID 22782401.
This indicates that subjects did not feel they were producing more power and consequently more heat. The authors concluded that the "safety switch" or the mechanisms existing in the body to prevent harmful effects are overridden by the drug administration (Roelands et al., 2008b). Taken together, these data indicate strong ergogenic effects of an increased DA concentration in the brain, without any change in the perception of effort.
- ^ a b c "Adderall XR- dextroamphetamine sulfate, dextroamphetamine saccharate, amphetamine sulfate and amphetamine aspartate capsule, extended release". DailyMed. Shire US Inc. 17 July 2019. Retrieved 22 December 2019.
- ^ a b c d e f g h Dolder PC, Strajhar P, Vizeli P, Hammann F, Odermatt A, Liechti ME (2017). "Pharmacokinetics and Pharmacodynamics of Lisdexamfetamine Compared with D-Amphetamine in Healthy Subjects". Front Pharmacol. 8: 617. doi:10.3389/fphar.2017.00617. PMC 5594082. PMID 28936175.
Inactive lisdexamfetamine is completely (>98%) converted to its active metabolite D-amphetamine in the circulation (Pennick, 2010; Sharman and Pennick, 2014). When lisdexamfetamine is misused intranasally or intravenously, the pharmacokinetics are similar to oral use (Jasinski and Krishnan, 2009b; Ermer et al., 2011), and the subjective effects are not enhanced by parenteral administration in contrast to D-amphetamine (Lile et al., 2011) thus reducing the risk of parenteral misuse of lisdexamfetamine compared with D-amphetamine. Intravenous lisdexamfetamine use also produced significantly lower increases in "drug liking" and "stimulant effects" compared with D-amphetamine in intravenous substance users (Jasinski and Krishnan, 2009a).
- ^ "Elvanse Adult 30mg Hard Capsules". Retrieved 26 February 2022.
2. Qualitative and quantitative composition. 30 mg Capsules: Each capsule contains 30 mg lisdexamfetamine dimesylate, equivalent to 8.9 mg of dexamfetamine. 50 mg Capsules: Each capsule contains 50 mg lisdexamfetamine dimesylate, equivalent to 14.8 mg of dexamfetamine. 70 mg Capsules: Each capsule contains 70 mg lisdexamfetamine dimesylate, equivalent to 20.8 mg of dexamfetamine.
- ^ Ermer J, Corcoran M, Lasseter K, Martin PT (December 2016). "Relative Bioavailabilities of Lisdexamfetamine Dimesylate and D-Amphetamine in Healthy Adults in an Open-Label, Randomized, Crossover Study After Mixing Lisdexamfetamine Dimesylate With Food or Drink". Ther Drug Monit. 38 (6): 769–776. doi:10.1097/FTD.0000000000000343. PMC 5158093. PMID 27661399.
- ^ Heedes G, Ailakis J. "Amphetamine (PIM 934)". INCHEM. International Programme on Chemical Safety. Retrieved 24 June 2014.
- ^ a b c d "Adderall XR- dextroamphetamine sulfate, dextroamphetamine saccharate, amphetamine sulfate and amphetamine aspartate capsule, extended release". DailyMed. 25 October 2023. Retrieved 18 March 2024.
- ^ a b Kooij JJ, Bijlenga D, Salerno L, Jaeschke R, Bitter I, Balázs J, et al. (February 2019). "Updated European Consensus Statement on diagnosis and treatment of adult ADHD". European Psychiatry. 56: 14–34. doi:10.1016/j.eurpsy.2018.11.001. hdl:10067/1564410151162165141. PMID 30453134. S2CID 53714228.
- ^ "Dexamphetamine tablets". Therapeutic Goods Administration. Retrieved 12 April 2014.
- ^ a b c Schoretsanitis G, de Leon J, Eap CB, Kane JM, Paulzen M (December 2019). "Clinically Significant Drug-Drug Interactions with Agents for Attention-Deficit/Hyperactivity Disorder". CNS Drugs. 33 (12): 1201–1222. doi:10.1007/s40263-019-00683-7. PMID 31776871. S2CID 208330108.
- ^ a b c d e f g Miller GM (January 2011). "The emerging role of trace amine-associated receptor 1 in the functional regulation of monoamine transporters and dopaminergic activity". Journal of Neurochemistry. 116 (2): 164–176. doi:10.1111/j.1471-4159.2010.07109.x. PMC 3005101. PMID 21073468.
- ^ a b c d Eiden LE, Weihe E (January 2011). "VMAT2: a dynamic regulator of brain monoaminergic neuronal function interacting with drugs of abuse". Annals of the New York Academy of Sciences. 1216 (1): 86–98. Bibcode:2011NYASA1216...86E. doi:10.1111/j.1749-6632.2010.05906.x. PMC 4183197. PMID 21272013.
VMAT2 is the CNS vesicular transporter for not only the biogenic amines DA, NE, EPI, 5-HT, and HIS, but likely also for the trace amines TYR, PEA, and thyronamine (THYR) ... [Trace aminergic] neurons in mammalian CNS would be identifiable as neurons expressing VMAT2 for storage, and the biosynthetic enzyme aromatic amino acid decarboxylase (AADC).
- ^ Sulzer D, Cragg SJ, Rice ME (August 2016). "Striatal dopamine neurotransmission: regulation of release and uptake". Basal Ganglia. 6 (3): 123–148. doi:10.1016/j.baga.2016.02.001. PMC 4850498. PMID 27141430.
Despite the challenges in determining synaptic vesicle pH, the proton gradient across the vesicle membrane is of fundamental importance for its function. Exposure of isolated catecholamine vesicles to protonophores collapses the pH gradient and rapidly redistributes transmitter from inside to outside the vesicle. ... Amphetamine and its derivatives like methamphetamine are weak base compounds that are the only widely used class of drugs known to elicit transmitter release by a non-exocytic mechanism. As substrates for both DAT and VMAT, amphetamines can be taken up to the cytosol and then sequestered in vesicles, where they act to collapse the vesicular pH gradient.
- ^ Ledonne A, Berretta N, Davoli A, Rizzo GR, Bernardi G, Mercuri NB (July 2011). "Electrophysiological effects of trace amines on mesencephalic dopaminergic neurons". Front. Syst. Neurosci. 5: 56. doi:10.3389/fnsys.2011.00056. PMC 3131148. PMID 21772817.
Three important new aspects of TAs action have recently emerged: (a) inhibition of firing due to increased release of dopamine; (b) reduction of D2 and GABAB receptor-mediated inhibitory responses (excitatory effects due to disinhibition); and (c) a direct TA1 receptor-mediated activation of GIRK channels which produce cell membrane hyperpolarization.
- ^ "TAAR1". GenAtlas. University of Paris. 28 January 2012. Retrieved 29 May 2014.
• tonically activates inwardly rectifying K(+) channels, which reduces the basal firing frequency of dopamine (DA) neurons of the ventral tegmental area (VTA)
- ^ Underhill SM, Wheeler DS, Li M, Watts SD, Ingram SL, Amara SG (July 2014). "Amphetamine modulates excitatory neurotransmission through endocytosis of the glutamate transporter EAAT3 in dopamine neurons". Neuron. 83 (2): 404–416. doi:10.1016/j.neuron.2014.05.043. PMC 4159050. PMID 25033183.
AMPH also increases intracellular calcium (Gnegy et al., 2004) that is associated with calmodulin/CamKII activation (Wei et al., 2007) and modulation and trafficking of the DAT (Fog et al., 2006; Sakrikar et al., 2012). ... For example, AMPH increases extracellular glutamate in various brain regions including the striatum, VTA and NAc (Del Arco et al., 1999; Kim et al., 1981; Mora and Porras, 1993; Xue et al., 1996), but it has not been established whether this change can be explained by increased synaptic release or by reduced clearance of glutamate. ... DHK-sensitive, EAAT2 uptake was not altered by AMPH (Figure 1A). The remaining glutamate transport in these midbrain cultures is likely mediated by EAAT3 and this component was significantly decreased by AMPH
- ^ Vaughan RA, Foster JD (September 2013). "Mechanisms of dopamine transporter regulation in normal and disease states". Trends Pharmacol. Sci. 34 (9): 489–496. doi:10.1016/j.tips.2013.07.005. PMC 3831354. PMID 23968642.
AMPH and METH also stimulate DA efflux, which is thought to be a crucial element in their addictive properties [80], although the mechanisms do not appear to be identical for each drug [81]. These processes are PKCβ– and CaMK–dependent [72, 82], and PKCβ knock-out mice display decreased AMPH-induced efflux that correlates with reduced AMPH-induced locomotion [72].
- ^ a b Wishart DS, Djombou Feunang Y, Guo AC, Lo EJ, Marcu A, Grant JR, et al. "Lisdexamfetamine | DrugBank Online". DrugBank. 5.0.
- ^ a b c Jasinski DR, Krishnan S (June 2009). "Abuse liability and safety of oral lisdexamfetamine dimesylate in individuals with a history of stimulant abuse". Journal of Psychopharmacology. 23 (4): 419–427. doi:10.1177/0269881109103113. PMID 19329547. S2CID 6138292.
- ^ Ermer J, Homolka R, Martin P, Buckwalter M, Purkayastha J, Roesch B (September 2010). "Lisdexamfetamine dimesylate: linear dose-proportionality, low intersubject and intrasubject variability, and safety in an open-label single-dose pharmacokinetic study in healthy adult volunteers". Journal of Clinical Pharmacology. 50 (9): 1001–1010. doi:10.1177/0091270009357346. PMID 20173084.
- ^ Strajhar P, Vizeli P, Patt M, Dolder PC, Kratschmar DV, Liechti ME, et al. (February 2019). "Effects of lisdexamfetamine on plasma steroid concentrations compared with d-amphetamine in healthy subjects: A randomized, double-blind, placebo-controlled study" (PDF). The Journal of Steroid Biochemistry and Molecular Biology. 186: 212–225. doi:10.1016/j.jsbmb.2018.10.016. PMID 30381248. S2CID 53183893.
- ^ Patel VB, Preedy VR, eds. (2022). Handbook of Substance Misuse and Addictions. Cham: Springer International Publishing. p. 2006. doi:10.1007/978-3-030-92392-1. ISBN 978-3-030-92391-4.
Amphetamine is usually consumed via inhalation or orally, either in the form of a racemic mixture (levoamphetamine and dextroamphetamine) or dextroamphetamine alone (Childress et al. 2019). In general, all amphetamines have high bioavailability when consumed orally, and in the specific case of amphetamine, 90% of the consumed dose is absorbed in the gastrointestinal tract, with no significant differences in the rate and extent of absorption between the two enantiomers (Carvalho et al. 2012; Childress et al. 2019). The onset of action occurs approximately 30 to 45 minutes after consumption, depending on the ingested dose and on the degree of purity or on the concomitant consumption of certain foods (European Monitoring Centre for Drugs and Drug Addiction 2021a; Steingard et al. 2019). It is described that those substances that promote acidification of the gastrointestinal tract cause a decrease in amphetamine absorption, while gastrointestinal alkalinization may be related to an increase in the compound's absorption (Markowitz and Patrick 2017).
- ^ a b c d e f g h i j k l m n "Adderall XR Prescribing Information" (PDF). United States Food and Drug Administration. Shire US Inc. December 2013. pp. 12–13. Retrieved 30 December 2013.
- ^ a b c d e "Metabolism/Pharmacokinetics". Amphetamine. Hazardous Substances Data Bank. United States National Library of Medicine – Toxicology Data Network. Archived from the original on 2 October 2017. Retrieved 2 October 2017.
Duration of effect varies depending on agent and urine pH. Excretion is enhanced in more acidic urine. Half-life is 7 to 34 hours and is, in part, dependent on urine pH (half-life is longer with alkaline urine). ... Amphetamines are distributed into most body tissues with high concentrations occurring in the brain and CSF. Amphetamine appears in the urine within about 3 hours following oral administration. ... Three days after a dose of (+ or -)-amphetamine, human subjects had excreted 91% of the (14)C in the urine
- ^ a b c d e "Vyvanse- lisdexamfetamine dimesylate capsule Vyvanse- lisdexamfetamine dimesylate tablet, chewable". DailyMed. Shire US Inc. 30 October 2019. Retrieved 22 December 2019.
- ^ a b c Santagati NA, Ferrara G, Marrazzo A, Ronsisvalle G (September 2002). "Simultaneous determination of amphetamine and one of its metabolites by HPLC with electrochemical detection". Journal of Pharmaceutical and Biomedical Analysis. 30 (2): 247–255. doi:10.1016/S0731-7085(02)00330-8. PMID 12191709.
- ^ "Compound Summary". p-Hydroxyamphetamine. PubChem Compound Database. United States National Library of Medicine – National Center for Biotechnology Information. Retrieved 15 October 2013.
- ^ "Compound Summary". p-Hydroxynorephedrine. PubChem Compound Database. United States National Library of Medicine – National Center for Biotechnology Information. Retrieved 15 October 2013.
- ^ "Compound Summary". Phenylpropanolamine. PubChem Compound Database. United States National Library of Medicine – National Center for Biotechnology Information. Retrieved 15 October 2013.
- ^ "Pharmacology and Biochemistry". Amphetamine. Pubchem Compound Database. United States National Library of Medicine – National Center for Biotechnology Information. Retrieved 12 October 2013.
- ^ a b Glennon RA (2013). "Phenylisopropylamine stimulants: amphetamine-related agents". In Lemke TL, Williams DA, Roche VF, Zito W (eds.). Foye's principles of medicinal chemistry (7th ed.). Philadelphia, US: Wolters Kluwer Health/Lippincott Williams & Wilkins. pp. 646–648. ISBN 9781609133450.
The simplest unsubstituted phenylisopropylamine, 1-phenyl-2-aminopropane, or amphetamine, serves as a common structural template for hallucinogens and psychostimulants. Amphetamine produces central stimulant, anorectic, and sympathomimetic actions, and it is the prototype member of this class (39). ... The phase 1 metabolism of amphetamine analogs is catalyzed by two systems: cytochrome P450 and flavin monooxygenase. ... Amphetamine can also undergo aromatic hydroxylation to p-hydroxyamphetamine. ... Subsequent oxidation at the benzylic position by DA β-hydroxylase affords p-hydroxynorephedrine. Alternatively, direct oxidation of amphetamine by DA β-hydroxylase can afford norephedrine.
- ^ Taylor KB (January 1974). "Dopamine-beta-hydroxylase. Stereochemical course of the reaction" (PDF). Journal of Biological Chemistry. 249 (2): 454–458. doi:10.1016/S0021-9258(19)43051-2. PMID 4809526. Retrieved 6 November 2014.
Dopamine-β-hydroxylase catalyzed the removal of the pro-R hydrogen atom and the production of 1-norephedrine, (2S,1R)-2-amino-1-hydroxyl-1-phenylpropane, from d-amphetamine.
- ^ Krueger SK, Williams DE (June 2005). "Mammalian flavin-containing monooxygenases: structure/function, genetic polymorphisms and role in drug metabolism". Pharmacology & Therapeutics. 106 (3): 357–387. doi:10.1016/j.pharmthera.2005.01.001. PMC 1828602. PMID 15922018.
Table 5: N-containing drugs and xenobiotics oxygenated by FMO - ^ Cashman JR, Xiong YN, Xu L, Janowsky A (March 1999). "N-oxygenation of amphetamine and methamphetamine by the human flavin-containing monooxygenase (form 3): role in bioactivation and detoxication". Journal of Pharmacology and Experimental Therapeutics. 288 (3): 1251–1260. PMID 10027866.
- ^ a b c Sjoerdsma A, von Studnitz W (April 1963). "Dopamine-beta-oxidase activity in man, using hydroxyamphetamine as substrate". British Journal of Pharmacology and Chemotherapy. 20 (2): 278–284. doi:10.1111/j.1476-5381.1963.tb01467.x. PMC 1703637. PMID 13977820.
Hydroxyamphetamine was administered orally to five human subjects ... Since conversion of hydroxyamphetamine to hydroxynorephedrine occurs in vitro by the action of dopamine-β-oxidase, a simple method is suggested for measuring the activity of this enzyme and the effect of its inhibitors in man. ... The lack of effect of administration of neomycin to one patient indicates that the hydroxylation occurs in body tissues. ... a major portion of the β-hydroxylation of hydroxyamphetamine occurs in non-adrenal tissue. Unfortunately, at the present time one cannot be completely certain that the hydroxylation of hydroxyamphetamine in vivo is accomplished by the same enzyme which converts dopamine to noradrenaline.
- ^ a b Badenhorst CP, van der Sluis R, Erasmus E, van Dijk AA (September 2013). "Glycine conjugation: importance in metabolism, the role of glycine N-acyltransferase, and factors that influence interindividual variation". Expert Opinion on Drug Metabolism & Toxicology. 9 (9): 1139–1153. doi:10.1517/17425255.2013.796929. PMID 23650932. S2CID 23738007.
Figure 1. Glycine conjugation of benzoic acid. The glycine conjugation pathway consists of two steps. First benzoate is ligated to CoASH to form the high-energy benzoyl-CoA thioester. This reaction is catalyzed by the HXM-A and HXM-B medium-chain acid:CoA ligases and requires energy in the form of ATP. ... The benzoyl-CoA is then conjugated to glycine by GLYAT to form hippuric acid, releasing CoASH. In addition to the factors listed in the boxes, the levels of ATP, CoASH, and glycine may influence the overall rate of the glycine conjugation pathway.
- ^ Horwitz D, Alexander RW, Lovenberg W, Keiser HR (May 1973). "Human serum dopamine-β-hydroxylase. Relationship to hypertension and sympathetic activity". Circulation Research. 32 (5): 594–599. doi:10.1161/01.RES.32.5.594. PMID 4713201. S2CID 28641000.
The biologic significance of the different levels of serum DβH activity was studied in two ways. First, in vivo ability to β-hydroxylate the synthetic substrate hydroxyamphetamine was compared in two subjects with low serum DβH activity and two subjects with average activity. ... In one study, hydroxyamphetamine (Paredrine), a synthetic substrate for DβH, was administered to subjects with either low or average levels of serum DβH activity. The percent of the drug hydroxylated to hydroxynorephedrine was comparable in all subjects (6.5-9.62) (Table 3).
- ^ Freeman JJ, Sulser F (December 1974). "Formation of p-hydroxynorephedrine in brain following intraventricular administration of p-hydroxyamphetamine". Neuropharmacology. 13 (12): 1187–1190. doi:10.1016/0028-3908(74)90069-0. PMID 4457764.
In species where aromatic hydroxylation of amphetamine is the major metabolic pathway, p-hydroxyamphetamine (POH) and p-hydroxynorephedrine (PHN) may contribute to the pharmacological profile of the parent drug. ... The location of the p-hydroxylation and β-hydroxylation reactions is important in species where aromatic hydroxylation of amphetamine is the predominant pathway of metabolism. Following systemic administration of amphetamine to rats, POH has been found in urine and in plasma.
The observed lack of a significant accumulation of PHN in brain following the intraventricular administration of (+)-amphetamine and the formation of appreciable amounts of PHN from (+)-POH in brain tissue in vivo supports the view that the aromatic hydroxylation of amphetamine following its systemic administration occurs predominantly in the periphery, and that POH is then transported through the blood-brain barrier, taken up by noradrenergic neurones in brain where (+)-POH is converted in the storage vesicles by dopamine β-hydroxylase to PHN. - ^ Matsuda LA, Hanson GR, Gibb JW (December 1989). "Neurochemical effects of amphetamine metabolites on central dopaminergic and serotonergic systems". Journal of Pharmacology and Experimental Therapeutics. 251 (3): 901–908. PMID 2600821.
The metabolism of p-OHA to p-OHNor is well documented and dopamine-β hydroxylase present in noradrenergic neurons could easily convert p-OHA to p-OHNor after intraventricular administration.
- ^ "Lisdexamfetamine". ChemSpider. Royal Society of Chemistry. 2015. Retrieved 22 April 2019.
- ^ Stahl PH, Wermuth DG, eds. (2011). Pharmaceutical Salts: Properties, Selection, and Use (2nd ed.). John Wiley & Sons. ISBN 978-3-906390-51-2.
- ^ "Molecular Weight Calculator". Lenntech. Retrieved 19 August 2015.
- ^ a b "Dextroamphetamine Sulfate USP". Mallinckrodt Pharmaceuticals. March 2014. Retrieved 19 August 2015.
- ^ a b "D-amphetamine sulfate". Tocris. 2015. Retrieved 19 August 2015.
- ^ a b "Amphetamine Sulfate USP". Mallinckrodt Pharmaceuticals. March 2014. Retrieved 19 August 2015.
- ^ "Dextroamphetamine Saccharate". Mallinckrodt Pharmaceuticals. March 2014. Retrieved 19 August 2015.
- ^ "Amphetamine Aspartate". Mallinckrodt Pharmaceuticals. March 2014. Retrieved 19 August 2015.
- ^ Mattingly G (May 2010). "Lisdexamfetamine dimesylate: a prodrug stimulant for the treatment of ADHD in children and adults". CNS Spectrums. 15 (5): 315–325. doi:10.1017/S1092852900027541. PMID 20448522. S2CID 46435024.
- ^ "Drug Approval Package: Vyvanse (Lisdexamfetamine Dimesylate) NDA #021977". U.S. Food and Drug Administration (FDA). Retrieved 18 March 2024.
- ^ "Summary Basis of Decision (SBD) for Vyvanse". Health Canada. 10 June 2010. Retrieved 18 March 2024.
- ^ "FDA expands uses of Vyvanse to treat binge-eating disorder". U.S. Food and Drug Administration (FDA) (Press release). 30 January 2015. Archived from the original on 26 January 2018. Retrieved 19 March 2023.
- ^ a b "Tentative approval" (PDF). 3 March 2023. Archived (PDF) from the original on 3 March 2023. Retrieved 24 April 2022.
- ^ "Canadian Patent Database / Base de données sur les brevets canadiens". www.ic.gc.ca. Retrieved 4 May 2023.
- ^ "DEA Office of Diversion Control" (PDF). DEA. Archived from the original (PDF) on 27 May 2016. Retrieved 7 November 2023.
- ^ Buoli M, Serati M, Cahn W (2016). "Alternative pharmacological strategies for adult ADHD treatment: a systematic review". Expert Review of Neurotherapeutics. 16 (2): 131–144. doi:10.1586/14737175.2016.1135735. PMID 26693882. S2CID 33004517.
- ^ "Lisdexamfetamine international brands". Drugs.com. Archived from the original on 11 November 2020. Retrieved 11 November 2020.
- ^ Rasmussen N (July 2006). "Making the first anti-depressant: amphetamine in American medicine, 1929-1950". J Hist Med Allied Sci. 61 (3): 288–323. doi:10.1093/jhmas/jrj039. PMID 16492800.
- ^ Brown AS, Gershon S (1993). "Dopamine and depression". J Neural Transm Gen Sect. 91 (2–3): 75–109. doi:10.1007/BF01245227. PMID 8099801.
- ^ Dale E, Bang-Andersen B, Sánchez C (May 2015). "Emerging mechanisms and treatments for depression beyond SSRIs and SNRIs". Biochemical Pharmacology. 95 (2): 81–97. doi:10.1016/j.bcp.2015.03.011. PMID 25813654.
- ^ Stotz G, Woggon B, Angst J (December 1999). "Psychostimulants in the therapy of treatment-resistant depression Review of the literature and findings from a retrospective study in 65 depressed patients". Dialogues in Clinical Neuroscience. 1 (3): 165–174. doi:10.31887/DCNS.1999.1.3/gstotz. PMC 3181580. PMID 22034135.
- ^ a b Nuñez NA, Joseph B, Pahwa M, Kumar R, Resendez MG, Prokop LJ, et al. (April 2022). "Augmentation strategies for treatment resistant major depression: A systematic review and network meta-analysis". Journal of Affective Disorders. 302: 385–400. doi:10.1016/j.jad.2021.12.134. PMC 9328668. PMID 34986373. S2CID 245657964.
- ^ Hirschler B (7 February 2014). "UPDATE 2-Shire scraps Vyvanse for depression after failed trials". Reuters. Archived from the original on 10 March 2016. Retrieved 13 February 2014.
- ^ "Lisdexamfetamine - Shionogi/Takeda". Adisinsight.springer.com. Retrieved 12 March 2022.
Clinical development is underway in the US, for mood disorders in children and adolescents for binge eating disorder and ADHD.
- ^ a b c d Giacobbe P, Rakita U, Lam R, Milev R, Kennedy SH, McIntyre RS (January 2018). "Efficacy and tolerability of lisdexamfetamine as an antidepressant augmentation strategy: A meta-analysis of randomized controlled trials". Journal of Affective Disorders. 226: 294–300. doi:10.1016/j.jad.2017.09.041. PMID 29028590.
- ^ Pan Z, Grovu RC, McIntyre RS (2019). "Translational Medicine Strategies in Drug Development for Mood Disorders". Translational Medicine in CNS Drug Development. Handbook of Behavioral Neuroscience. Vol. 29. Elsevier. pp. 333–347. doi:10.1016/B978-0-12-803161-2.00023-0. ISBN 978-0-12-803161-2. ISSN 1569-7339. S2CID 196561249.
- ^ Madhoo M, Keefe RS, Roth RM, Sambunaris A, Wu J, Trivedi MH, et al. (May 2014). "Lisdexamfetamine dimesylate augmentation in adults with persistent executive dysfunction after partial or full remission of major depressive disorder". Neuropsychopharmacology. 39 (6): 1388–1398. doi:10.1038/npp.2013.334. PMC 3988542. PMID 24309905.