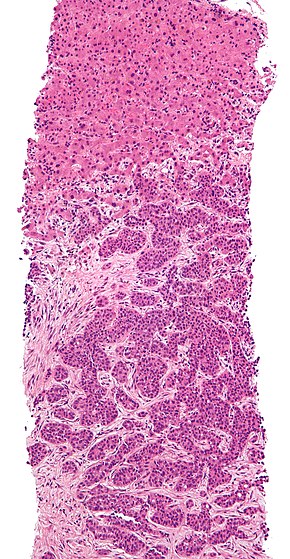
Liver biopsy is the biopsy (removal of a small sample of tissue) from the liver. It is a medical test that is done to aid diagnosis of liver disease, to assess the severity of known liver disease, and to monitor the progress of treatment.[1]
| Liver biopsy | |
|---|---|
 | |
| ICD-9-CM | 50.1 |
| MedlinePlus | 003895 |
Medical uses
editLiver biopsy is often required for the diagnosis of a liver problem (jaundice, abnormal blood tests) where blood tests, such as hepatitis A serology, have not been able to identify a cause. It is also required if hepatitis is possibly the result of medication, but the exact nature of the reaction is unclear. Alcoholic liver disease and tuberculosis of the liver may be diagnosed through biopsy.[1] Direct biopsy of tumors of the liver may aid the diagnosis, although this may be avoided if the source is clear (e.g. spread from previously known colorectal cancer).[1] Liver biopsy will likely remain particularly important in the diagnosis of unexplained liver disease. Non-invasive tests for liver fibrosis in alcoholic, nonalcoholic and viral liver diseases are likely to become more widely used.[2]
If the diagnosis is already clear, such as chronic hepatitis B or hepatitis C, liver biopsy is useful to assess the severity of the associated liver damage. The same is true for haemochromatosis (iron overload), although it is frequently omitted. Primary biliary cirrhosis and primary sclerosing cholangitis may require biopsy, although other diagnostic modalities have made this less necessary.[1]
Occasionally, liver biopsy is required to monitor the progress of treatment, such as in chronic viral hepatitis.[1] It is an effective way to measure changes in the Ishak fibrosis score.[3]
For the last century liver biopsy has been considered as the gold standard for assessing the stage and the grade of chronic liver disease. Consensus conference statements recommended liver biopsy in the management of almost all patients with hepatitis C and B.[citation needed]
Biopsy results show significant variability (up to 40% for fibrosis diagnosis) which can lead to a wrong diagnosis. The result depends on the representativity of the punctured sample.[4]
Only 5% of patients at risk of fibrosis have liver biopsy. In 2002, the consensus conferences in France and in the USA raised the possibility of treating patients with chronic hepatitis without liver biopsy.[5][6] These conferences also underlined the necessity of developing reliable non-invasive tests that might be an alternative to liver biopsy both in hepatitis B and C.
Risks and limitations
editLiver biopsy is generally a safe procedure, but it is invasive. Complications of liver biopsy are rare but potentially lethal.[7] The majority of complications (60%) occur within two hours, and 96% occur within 24 hours following the procedure.[7] Approximately 2–3% of patients undergoing liver biopsy require hospitalization for the management of an adverse event.[8][9] Thirty percent of patients experience significant pain during the procedure.[10]
Significant bleeding after a liver biopsy occurs in 1–2 out of 100 patients who are biopsied.[11][12] Bleeding usually becomes apparent within three to four hours. It often stops on its own, but if it persists, a blood transfusion may be needed. Surgery or angiography (a procedure in which the bleeding site is identified and treated) may be required if the bleeding is severe or does not stop on its own. Intraperitoneal hemorrhage is the most serious consequence of bleeding. Fatal complications have been reported in up to 0.01–0.3% of biopsied patients.[12][13][14]
Procedure and variants
editLiver biopsies may be taken percutaneously (via a needle through the skin), transvenously (through the blood vessels), endoscopically (through endoscopic ultrasound fine needle biopsy), or directly during abdominal surgery. The sample is examined by microscope, and may be processed further by immunohistochemistry, determination of iron and copper content, and microbiological culture if tuberculosis is suspected[15]
For a percutaneous biopsy, it is recommended to use a Birmingham gauge 16 or wider cutting needle, and obtaining a length of 20–25 mm of liver tissue. The presence of 10–12 portal tracts within the specimen is considered sufficient for reliable analysis, ensuring that architectural relationships between structures are maintained.[16]
Liver biopsy results are limited by sampling error,[10] as abnormal findings may be missed if only normal tissue is retrieved. In addition, interpretation of liver biopsy results may vary.[10]
History
editThe first liver aspirate was performed by the German physician Paul Ehrlich in 1883. In 1923, the first report of percutaneous liver biopsy was described.[1][10] The transjugular approach was pioneered by radiologist Charles Dotter in the 1970s.[17]
Non-invasive alternatives
editNon-invasive alternatives to liver biopsy in hepatitis C patients include both functional staging (quantitative liver function tests) and determination of fibrosis from non-invasive tests. These latter tests are described below and share the disadvantage of estimating fibrosis rather than function. Functional staging has the advantage of evaluating the whole liver and directly measuring hepatic function that determines many clinical outcomes.[18] The ability to predict clinical outcomes is the best proof of the value of a clinical test. Quantitative hepatic function tests were better than combinations of routine blood tests and Ishak fibrosis score in predicting clinical outcomes. The best of these were the perfused hepatic mass (PHM) by quantitative laparoscopic liver spleen scan (QLSS) and oral Cholate clearance and shunt, a blood test. The QLSS measurement of spleen volume per ideal body weight was nearly as good.[18]
Multiphasic MRI is useful in diagnosing various types of liver lesions such as hepatocellular carcinoma, cholangiocarcinoma, hepatocellular adenoma, focal nodular hyperplasia, and hemangioma.[19]
FibroTest (FibroSure in the USA) and FibroMax are non-invasive tests using a blood sample and an algorithm. The test results correspond to stages F0-F4 and grades A0-A3 of the METAVIR scoring system.[20] In 2007 FibroTest was validated by French Health Authorities as a first-line diagnosis of liver injury before biopsy. It was recommended to be a better predictor than biopsy staging for hepatitis C complications and death.[21]
FibroScan is a type of ultrasound machine that uses transient elastography to measure liver stiffness. Its diagnostic performance for fibrosis is similar to that of methods based on serologic markers. Combined use of Fibroscan and Fibrotest could avoid a liver biopsy in most patients with chronic hepatitis C.[22] Other ultrasonic techniques used to characterize liver stiffness include Acoustic Radiation Force Impulse (ARFI) Imaging.[23]
Hepascore is a blood test developed in Australia combining the following clinical and laboratory variables: age, gender, bilirubin, GGT, hyaluronic acid, alpha 2 macroglobin to create a score. The test has been validated for patients with hepatitis B,[24] hepatitis C[25] and non-alcoholic fatty liver disease.[26]
APRI (AST to platelet ratio index) is a quick serum biomarker for fibrosis assessment from Italy. This simple index is made up of routine laboratory tests. The test has not been validated by any health authorities. 50% of the results are unclassifiable. APRI may be useful for excluding significant fibrosis in hepatitis C.[citation needed]
References
edit- ^ a b c d e f Grant A, Neuberger J (October 1999). "Guidelines on the use of liver biopsy in clinical practice". Gut. 45 (Suppl 4): IV1–IV11. doi:10.1136/gut.45.2008.iv1. PMC 1766696. PMID 10485854.
- ^ Manning DS, Afdhal NH (May 2008). "Diagnosis and quantitation of fibrosis". Gastroenterology. 134 (6): 1670–81. CiteSeerX 10.1.1.464.1263. doi:10.1053/j.gastro.2008.03.001. PMID 18471546.
- ^ Hoefs, JC; Shiffman, ML; Goodman, ZD; Kleiner, DE; Dienstag, JL; Stoddard, AM; HALT-C Trial, Group. (September 2011). "Rate of progression of hepatic fibrosis in patients with chronic hepatitis C: results from the HALT-C Trial". Gastroenterology. 141 (3): 900–908.e1–2. doi:10.1053/j.gastro.2011.06.007. PMC 3773843. PMID 21699796.
- ^ Regev A, Berho M, Jeffers LJ, et al. (October 2002). "Sampling error and intraobserver variation in liver biopsy in patients with chronic HCV infection". Am. J. Gastroenterol. 97 (10): 2614–8. doi:10.1111/j.1572-0241.2002.06038.x. PMID 12385448. S2CID 25506596.[dead link]
- ^ Agence Nationale d'Accréditation et d'Evaluation en Santé (ANAES) (April 2002). "Consensus conference. Treatment of hepatitis C". Gastroenterol. Clin. Biol. 26 (Spec No 2): B303–20. PMID 12180305.
- ^ <Please add first missing authors to populate metadata.> (November 2002). "Recommendations from the National Institutes of Health consensus development conference statement: management of hepatitis C: 2002". Hepatology. 36 (5): 1039. doi:10.1002/hep.510360502. PMID 12395309.
- ^ a b Diagnostic Liver Biopsy at eMedicine
- ^ Janes; Lindor, KD (1993). "Outcome of patients hospitalized for complications after outpatient liver biopsy". Ann Intern Med. 118 (2): 96–8. doi:10.7326/0003-4819-118-2-199301150-00003. PMID 8416324. S2CID 37740050.
- ^ Pasha; et al. (1998). "Cost-effectiveness of ultrasound-guided liver biopsy". Hepatology. 27 (5): 1220–6. doi:10.1002/hep.510270506. PMID 9581674.
- ^ a b c d Lim, JK; Flamm, SL; Singh, S; Falck-Ytter, YT; Clinical Guidelines Committee of the American Gastroenterological, Association. (May 2017). "American Gastroenterological Association Institute Guideline on the Role of Elastography in the Evaluation of Liver Fibrosis". Gastroenterology. 152 (6): 1536–1543. doi:10.1053/j.gastro.2017.03.017. PMID 28442119.
- ^ "Liver Biopsy: Learn How This Procedure Is Performed". medicinenet.com. Retrieved 22 April 2018.
- ^ a b Gilmore; et al. (1995). "Indications, methods, and outcomes of percutaneous liver biopsy in England and Wales: an audit by the British Society of Gastroenterology and the Royal College of Physicians of London". Gut. 36 (3): 437–41. doi:10.1136/gut.36.3.437. PMC 1382461. PMID 7698705.
- ^ Strassburg; Manns, MP (2006). "Approaches to liver biopsy techniques-revisited". Semin Liver Dis. 26 (4): 318–27. doi:10.1055/s-2006-951599. PMID 17051446. S2CID 260320814.
- ^ Froehlich; et al. (1993). "Practice and complications of liver biopsy. Results of a nationwide survey in Switzerland". Dig Dis Sci. 38 (8): 1480–4. doi:10.1007/bf01308607. PMID 8344104. S2CID 21781162.
- ^ Silva MA, Hegab B, Hyde C, Guo B, Buckels JA, Mirza DF (November 2008). "Needle track seeding following biopsy of liver lesions in the diagnosis of hepatocellular cancer: a systematic review and meta-analysis". Gut. 57 (11): 1592–6. doi:10.1136/gut.2008.149062. PMID 18669577. S2CID 20355451.
- ^ Boyd, Alexander; Cain, Owen; Chauhan, Abhishek; Webb, Gwilym James (2020). "Medical liver biopsy: background, indications, procedure and histopathology". Frontline Gastroenterology. 11 (1): 40–47. doi:10.1136/flgastro-2018-101139. ISSN 2041-4137. PMC 6914302. PMID 31885839.
- ^ Rösch J, Lakin PC, Antonovic R, Dotter CT (August 1973). "Transjugular approach to liver biopsy and transhepatic cholangiography". N. Engl. J. Med. 289 (5): 227–31. doi:10.1056/NEJM197308022890501. PMID 4713761.
- ^ a b Gregory T Everson, Mitchell L Shiffman, John C Hoefs, Timothy R Morgan, Richard K Sterling, David A Wagner, Shannon Lauriski, Teresa M Curto, Anne Stoddard, Elizabeth C Wright Quantitative liver function tests improve the prediction of clinical outcomes in chronic hepatitis C: results from the Hepatitis C Antiviral Long-term Treatment Against Cirrhosis Trial. 2011 Hepatology 55(4):1019-29
- ^ Tapper, Elliot B.; Lok, Anna S.-F. (2017-08-24). Longo, Dan L. (ed.). "Use of Liver Imaging and Biopsy in Clinical Practice". New England Journal of Medicine. 377 (8): 756–768. doi:10.1056/NEJMra1610570. ISSN 0028-4793. PMID 28834467. S2CID 205117722.
- ^ "Scientific Publications". 2008-10-18. Archived from the original on 2008-10-18.
- ^ Poynard T, Imbert-Bismut F, Munteanu M, et al. (2004). "Overview of the diagnostic value of biochemical markers of liver fibrosis (FibroTest, HCV FibroSure) and necrosis (ActiTest) in patients with chronic hepatitis C". Comp Hepatol. 3 (1): 8. doi:10.1186/1476-5926-3-8. PMC 522750. PMID 15387887.
- ^ Castéra L, Vergniol J, Foucher J, et al. (February 2005). "Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C". Gastroenterology. 128 (2): 343–50. doi:10.1053/j.gastro.2004.11.018. PMID 15685546.
- ^ Yoneda M, Suzuki K, Kato S, et al. (August 2010). "Nonalcoholic fatty liver disease: US-based acoustic radiation force impulse elastography". Radiology. 256 (2): 640–7. doi:10.1148/radiol.10091662. PMID 20529989.
- ^ Adams LA, Bulsara M, Rossi E, DeBoer B, Speers D, George J, Kench J, Farrell G, McCaughan GW, Jeffrey GP (October 2005). "Hepascore – An Accurate Validated Predictor of Liver Fibrosis in Chronic Hepatitis C Infection". Clinical Chemistry. 51 (10): 1867–73. doi:10.1373/clinchem.2005.048389. PMID 16055434.
- ^ Raftopoulos SC, George J, Bourliere M, Rossi E, de Boer WB, Jeffrey GP, Bulsara M, Speers DJ, Macquillan G, Ching HL, Kontorinis N, Cheng W, Flexman J, Fermoyle S, Rigby P, Walsh L, McLeod D, Adams LA (April 2012). "Comparison of noninvasive models of fibrosis in chronic hepatitis B". Hepatology International. 6 (2): 457–467. doi:10.1007/s12072-011-9296-5. PMID 21748376. S2CID 22215786.
- ^ Adams LA, George J, Bugianesi E, Rossi E, De Boer WB, van der Poorten D, Ching HL, Bulsara M, Jeffrey GP (October 2011). "Complex non-invasive fibrosis models are more accurate than simple models in non-alcoholic fatty liver disease". Journal of Gastroenterology and Hepatology. 26 (10): 1536–43. doi:10.1111/j.1440-1746.2011.06774.x. PMID 21950746. S2CID 205467096.