Pentylenetetrazol (PTZ), also known as pentylenetetrazole, leptazol, metrazol, pentetrazol (INN), pentamethylenetetrazol, Corazol, Cardiazol, or Deumacard, is a drug formerly used as a circulatory and respiratory stimulant. High doses cause convulsions, as discovered by Hungarian-American neurologist and psychiatrist Ladislas J. Meduna in 1934. It has been used in convulsive therapy, and was found to be effective—primarily for depression—but side effects such as uncontrolled seizures were difficult to avoid.[1] In 1939, pentylenetetrazol was replaced by electroconvulsive therapy, which is easier to administer, as the preferred method for inducing seizures in England's mental hospitals. In the US, its approval by the Food and Drug Administration was revoked in 1982.[2] It is used in Italy as a cardio-respiratory stimulant in combination with codeine in a cough suppressant drug.[3]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Metrazol, others |
| Other names | PTZ; Pentylenetetrazole; Leptazol; Metrazol; Pentetrazol; Pentamethylenetetrazol |
| ATC code | |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.200 |
| Chemical and physical data | |
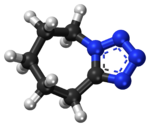
| Formula | C6H10N4 |
| Molar mass | 138.174 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Side effects
editPentylenetetrazol is anxiogenic and has been known to induce severe anxiety in humans.[4]
Mechanism
editThe mechanism of pentylenetetrazol is not well understood, and it may have multiple mechanisms of action. In 1984, Squires et al. published a report analyzing pentylenetetrazol and several structurally related convulsant drugs. They found that in vivo convulsant potency was strongly correlated to in vitro affinity to the picrotoxin binding site on the GABA-A receptor complex. Many GABA-A ligands, such as the sedatives diazepam and phenobarbital, are effective anticonvulsants, but presumably pentylenetetrazol has the opposite effect when it binds to the GABA-A receptor.[5]
Several studies have focused on the way pentylenetetrazol influences neuronal ion channels. A 1987 study found that pentylenetetrazol increases calcium influx and sodium influx, both of which depolarize the neuron. Because these effects were antagonized by calcium channel blockers, pentylenetetrazol apparently acts at calcium channels, and it causes them to lose selectivity and conduct sodium ions, as well.[6]
Research
editPentylenetetrazol has been used experimentally to study seizure phenomena and to identify pharmaceuticals that may control seizure susceptibility. For instance, researchers can induce status epilepticus in animal models. Pentylenetetrazol is also a prototypical anxiogenic drug and has been extensively used in animal models of anxiety. Pentylenetetrazol produces a reliable discriminative stimulus, which is largely mediated by the GABAA receptor. Several classes of compounds can modulate the pentylenetetrazol discriminative stimulus, including 5-HT1A, 5-HT3, NMDA, glycine, and L-type calcium channel ligands.[7]
Pentylenetetrazol is being studied as a wakefulness-promoting agent in the treatment of idiopathic hypersomnia and narcolepsy.[8][9]
See also
editReferences
edit- ^ Read CF (1940). "Consequences of metrazol shock therapy". American Journal of Psychiatry. 97 (3): 667–76. doi:10.1176/ajp.97.3.667.
- ^ Minkel JR (February 25, 2007). "Drug May Counteract Down Syndrome". Scientific American. Retrieved 2007-03-20.
- ^ "Cardiazol-Paracodina". Agenzia Italiana del Farmaco.
- ^ Durant C, Christmas D, Nutt D (2009). "The Pharmacology of Anxiety". Current Topics in Behavioral Neurosciences. Berlin, Heidelberg: Springer Berlin Heidelberg. p. 303–330. doi:10.1007/7854_2009_8. ISBN 978-3-642-02911-0. ISSN 1866-3370.
Preliminary evidence that reducing GABAergic transmission induces anxiety came from the early use of pentylenetetrazol (PTZ) a convulsant drug used to induce seizures in the treatment of severe psychiatric disorders before the discovery of ECT. During its use dose titration was difficult, in many cases too little was given and no seizure was caused. This, however, produced a severely anxious state, leading to patients feeling 'as if they were going to die', and trying (often successfully) to escape from the clinic. Memory of this anxiety was extremely strong resulting in resistance to return to therapy and it was later shown that PTZ acts as an antagonist GABAA receptor.
- ^ Squires RF, Saederup E, Crawley JN, Skolnick P, Paul SM (October 1984). "Convulsant potencies of tetrazoles are highly correlated with actions on GABA/benzodiazepine/picrotoxin receptor complexes in brain". Life Sciences. 35 (14): 1439–1444. doi:10.1016/0024-3205(84)90159-0. PMID 6090836.
- ^ Papp A, Fehér O, Erdélyi L (1987). "The ionic mechanism of the pentylenetetrazol convulsions". Acta Biologica Hungarica. 38 (3–4): 349–361. PMID 3503442.
- ^ Jung ME, Lal H, Gatch MB (June 2002). "The discriminative stimulus effects of pentylenetetrazol as a model of anxiety: recent developments". Neuroscience and Biobehavioral Reviews. 26 (4): 429–439. doi:10.1016/S0149-7634(02)00010-6. PMID 12204190. S2CID 26055062.
- ^ "Pentylenetetrazole - Balance Therapeutics". AdisInsight. Springer Nature Switzerland AG. 28 June 2020. Retrieved 25 September 2024.
- ^ Takahashi T, Noriaki S, Matsumura M, Li C, Takahashi K, Nishino S (3 October 2018). "Advances in pharmaceutical treatment options for narcolepsy". Expert Opinion on Orphan Drugs. 6 (10): 597–610. doi:10.1080/21678707.2018.1521267. ISSN 2167-8707.