Tafenoquine, sold under the brand name Krintafel among others, is a medication used to prevent and to treat malaria.[3] With respect to acute malaria, it is used together with other medications to prevent relapse by Plasmodium vivax.[3] It may be used to prevent all types of malaria.[3] It is taken by mouth.[4]
 | |
| Clinical data | |
|---|---|
| Pronunciation | ta fen' oh kwin |
| Trade names | Krintafel, Arakoda, others |
| Other names | Etaquine,[1] WR 238605,[1] SB-252263 |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a618050 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth |
| Drug class | Antimalarial |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| NIAID ChemDB | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
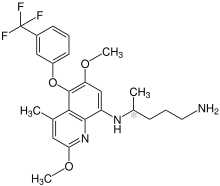
| Formula | C24H28F3N3O3 |
| Molar mass | 463.501 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Common side effects include vomiting, headache, and dizziness.[4] Other side effects may include methemoglobinemia, trouble sleeping, and anaphylaxis.[4] In people with G6PD deficiency, red blood cell breakdown may occur.[4] Use in pregnancy is not recommended.[4] Tafenoquine is in the 8-aminoquinoline family of medications.[3] The mechanism of action is unclear but it is effective both in the liver and bloodstream.[4][3] A possible mechanism of action and other novel perspectives have been published.[5]
Tafenoquine was approved for medical use in Australia and in the United States in 2018.[3][6] Tafenoquine is related to primaquine.[7]
Medical use
editPrevention
editTafenoquine may be used to prevent all types of malaria.[3] For this use 200 mg 3 days before travel then 200 mg per week until one week after travel is recommended.[7]
Treatment
editTafenoquine is used for eliminating the hypnozoite stage of Plasmodium vivax and Plasmodium ovale that is responsible for relapse of these malarial infections, even when the blood stages are successfully cleared. Primaquine for 14 days can also be used for this. The advantage of tafenoquine is that it has a long half-life (2–3 weeks) and therefore a single treatment is sufficient.[8] For this use, a single dose of 300 mg is recommended.[7] It is used with another medication, such as chloroquine, that kills the parasites in the bloodstream.[9]
There is a need to determine whether or not tafenoquine kills the numerous, non-circulating asexual P. vivax parasites that are now known to occur in the spleen, bone marrow, and possibly elsewhere in chronic infections.[10][11]
Chemistry
editTafenoquine contains a stereocenter and consists of two enantiomers. This is a mixture of (R) - and the (S) - Form:
| Enantiomers of tafenoquine | |
|---|---|
| (R)-Form |
(S)-Form |
History
editTafenoquine was approved for medical use in Australia and in the United States in 2018.[3][6] Tafenoquine was given an orphan drug designation and was granted breakthrough therapy status in 2013 in the United States.[12][13]
Society and culture
editOne version is made by GlaxoSmithKline.[4] While another is made by 60 Degrees Pharmaceutical.[14]
Names
editEtaquine was a generic name proposed by WRAIR, and subsequently rejected by CDER.[citation needed]
Trade names
References
edit- ^ a b Peters W (July 1999). "The evolution of tafenoquine--antimalarial for a new millennium?". Journal of the Royal Society of Medicine. 92 (7): 345–352. doi:10.1177/014107689909200705. PMC 1297286. PMID 10615272.
- ^ Use During Pregnancy and Breastfeeding
- ^ a b c d e f g h Haston JC, Hwang J, Tan KR (November 2019). "Guidance for Using Tafenoquine for Prevention and Antirelapse Therapy for Malaria - United States, 2019". MMWR. Morbidity and Mortality Weekly Report. 68 (46): 1062–1068. doi:10.15585/mmwr.mm6846a4. PMC 6871897. PMID 31751320.
- ^ a b c d e f g "Tafenoquine Succinate (Krintafel) Monograph for Professionals". Drugs.com. Retrieved 22 November 2019.
- ^ Markus MB (2021). "Safety and Efficacy of Tafenoquine for Plasmodium vivax Malaria Prophylaxis and Radical Cure: Overview and Perspectives". Therapeutics and Clinical Risk Management. 17: 989–999. doi:10.2147/TCRM.S269336. PMC 8435617. PMID 34526770.
- ^ a b Hounkpatin AB, Kreidenweiss A, Held J (March 2019). "Clinical utility of tafenoquine in the prevention of relapse of Plasmodium vivax malaria: a review on the mode of action and emerging trial data". Infection and Drug Resistance. 12: 553–570. doi:10.2147/IDR.S151031. PMC 6411314. PMID 30881061.
- ^ a b c "Tafenoquine Approved for Malaria Prophylaxis and Treatment". Centers for Disease Control and Prevention (CDC). 25 April 2019. Retrieved 22 November 2019.
- ^ Elmes NJ, Nasveld PE, Kitchener SJ, Kocisko DA, Edstein MD (November 2008). "The efficacy and tolerability of three different regimens of tafenoquine versus primaquine for post-exposure prophylaxis of Plasmodium vivax malaria in the Southwest Pacific". Transactions of the Royal Society of Tropical Medicine and Hygiene. 102 (11): 1095–1101. doi:10.1016/j.trstmh.2008.04.024. PMID 18541280.
- ^ "Conclusions and Recommendations from the Fifteenth Meeting of the WHO Advisory Committee on Safety of Medicinal Products (ACSoMP)" (PDF). WHO. Retrieved 22 November 2019.
- ^ Markus MB (November 2019). "Killing of Plasmodium vivax by Primaquine and Tafenoquine". Trends in Parasitology. 35 (11): 857–859. doi:10.1016/j.pt.2019.08.009. PMID 31522991. S2CID 202582476.
- ^ Markus MB (May 2023). "Putative Contribution of 8-Aminoquinolines to Preventing Recrudescence of Malaria". Tropical Medicine and Infectious Disease. 8 (5): 278. doi:10.3390/tropicalmed8050278. PMC 10223033. PMID 37235326.
- ^ "Krintafel (tafenoquine succinate tablets) FDA Advisory Committee Briefing Document" (PDF). Food and Drug Administration. 12 July 2018. Archived from the original on 23 November 2019. Retrieved 22 November 2019.
- ^ "Krintafel Orphan Drug Designation and Approval". U.S. Food and Drug Administration (FDA). Archived from the original on 23 November 2019. Retrieved 22 November 2019.
- ^ Tan KR, Hwang J (January 2018). "Tafenoquine receives regulatory approval in USA for prophylaxis of malaria and radical cure of Plasmodium vivax". Journal of Travel Medicine. 25 (1). doi:10.1093/jtm/tay071. PMC 10956546. PMID 30137454.
- ^ "Kozenis (tafenoquine) approved by the Australian Therapeutic Goods Administration for the radical cure of P. vivax malaria" (Press release). Medicines for Malaria Venture. 21 September 2018. Retrieved 15 October 2018.
- ^ "Kodatef". NPS MedicineWise. 17 May 2022.
- ^ "Drug Approval Package: Arakoda". U.S. Food and Drug Administration (FDA). 13 February 2019. Archived from the original on 23 November 2019. Retrieved 22 November 2019.
- ^ "Drug Approval Package: Krintafel (tafenoquine)". U.S. Food and Drug Administration (FDA). 24 August 2018. Archived from the original on 23 November 2019. Retrieved 22 November 2019.
- ^ "Drug Trials Snapshots: Krintafel". U.S. Food and Drug Administration (FDA). 6 August 2018. Archived from the original on 23 November 2019. Retrieved 22 November 2019.
- ^ "US FDA approves Krintafel (tafenoquine) for the radical cure of P. vivax malaria" (Press release). Medicines for Malaria Venture. 20 July 2018. Retrieved 15 October 2018.
External links
edit- "Tafenoquine". Drug Information Portal. U.S. National Library of Medicine.