| Submission declined on 6 November 2024 by I dream of horses (talk). This submission is not adequately supported by reliable sources. Reliable sources are required so that information can be verified. If you need help with referencing, please see Referencing for beginners and Citing sources.
Where to get help
How to improve a draft
You can also browse Wikipedia:Featured articles and Wikipedia:Good articles to find examples of Wikipedia's best writing on topics similar to your proposed article. Improving your odds of a speedy review To improve your odds of a faster review, tag your draft with relevant WikiProject tags using the button below. This will let reviewers know a new draft has been submitted in their area of interest. For instance, if you wrote about a female astronomer, you would want to add the Biography, Astronomy, and Women scientists tags. Editor resources
|  |
 Comment: Has standard "wall of text" issues including potentially time-consuming issues with formatting, and little sourcing per-capita. I dream of horses (Hoofprints) (Neigh at me) 08:22, 6 November 2024 (UTC)
Comment: Has standard "wall of text" issues including potentially time-consuming issues with formatting, and little sourcing per-capita. I dream of horses (Hoofprints) (Neigh at me) 08:22, 6 November 2024 (UTC)
Terson's syndrome is a condition where eye haemorrhages occur due to intracranial bleeding, most often associated with subarachnoid haemorrhage (SAH), commonly from a ruptured cerebral aneurysm. Patients may experience blurred vision, floaters, or complete vision loss due to retinal or vitreous haemorrhage, and neurological symptoms like severe headaches, nausea, seizures, and confusion may also arise. Diagnosis is challenging as the eye bleeding can resemble other conditions, such as diabetic retinopathy or retinal vein occlusion. A fundoscopic exam is the primary diagnostic method, but imaging like CT, MRI, and OCT can aid in confirming the diagnosis. Treatment involves managing intracranial pressure and haemorrhage, with options like vitrectomy or anti-VEGF injections for persistent eye bleeds. The prognosis depends on the severity of both neurological and ocular damage, with early intervention improving recovery chances. However, recurrence risks exist depending on the underlying cause of the haemorrhage. Research continues on improving early diagnosis, surgical approaches, and understanding the genetic and molecular factors influencing the disease.
History of the Disease: An instance of intraretinal hemorrhage coexisting with subarachnoid hemorrhage (SAH) was initially documented by German ophthalmologist Moritz Litten in 1881. Later, in 1900, French ophthalmologist Albert Terson reported a link between SAH—later known as Terson syndrome—and vitreous hemorrhage. This syndrome includes many kinds of intraocular hemorrhages, usually caused by a sudden increase in intracranial pressure (ICP), which can happen in combination with SAH, intracerebral hemorrhage, or traumatic brain injury.
The vitreous, sub-hyaloid, subretinal space, intraretinal regions, or beneath the internal limiting membrane are some of the locations where the hemorrhages may occur in the eye. According to Dr. Hayreh, the rupture of capillaries in the optic nerve, which is most likely brought on by elevated retinal venous pressure from central retinal vein compression, is the source of these retinal hemorrhages. The intricate vascular connections between the brain and the eye are highlighted by the fact that Terson syndrome is most frequently observed after aneurysmal subarachnoid hemorrhages. This emphasizes how crucial it is to diagnose and treat the illness using a thorough, interdisciplinary approach. Terson syndrome occurs in about 13% of SAH patients, especially in more severe instances (shown by a higher Hunt-Hess score), and these cases are linked to a higher risk of death.
Signs and Symptoms: The severity of the vision-related problems that people with Terson syndrome encounter varies greatly. The main symptom, which frequently affects one or both eyes, is an abrupt loss of vision or blurred vision brought on by bleeding in the vitreous cavity, which is the gel-like region that fills most of the eye. The degree of vision impairment in the affected eye can range from slight blurriness to total blindness, depending on the blood volume.
Additional symptoms could include light sensitivity and floaters, which are small dots or forms that appear to move across the visual field. Some individuals may not immediately notice changes in their vision if the bleeding is minor or just affects one eye. However, visual impairments are usually more obvious and can significantly affect daily activities when both eyes are affected.Severe neurological events, especially subarachnoid hemorrhage (bleeding around the brain) or elevated intracranial pressure, are frequently linked to Terson syndrome. Because of this, people may also have symptoms associated with certain brain disorders, such as severe headaches, nausea, vomiting, or stiff necks, which may come before visual problems and act as early warning indicators.
Although there is proof that brain bleeding and eye hemorrhage are related, it is still unknown why some people have Terson syndrome and others do not. More study is necessary to identify at-risk patients since the exact reason why increased brain pressure can sometimes result in ruptured blood vessels in the eye is still unclear. Additionally, even though treating eye hemorrhages can enhance vision, the long-term effects are still unknown, particularly if the diagnosis is delayed. A comprehensive assessment of the brain and eye is necessary to diagnose Terson syndrome. Optical Coherence Tomography (OCT) offers precise cross-sectional images of the retina to verify the existence of hemorrhage, whereas fundoscopy is frequently utilized to find bleeding in the vitreous cavity or on the retina.
An eye ultrasound can assist in visualizing internal bleeding when eye bleeding is suspected but not yet visible. Brain imaging using CT or MRI scans is usually done to look for underlying cerebral hemorrhage or high pressure within the skull because Terson syndrome is frequently associated with serious brain diseases including subarachnoid hemorrhage.
The standard diagnostic criteria and methods
Terson's syndrome is frequently diagnosed by combining neurological and ophthalmological testing. Fundoscopy, which enables direct evaluation of the retina for indications of bleeding, usually in the vitreous or retinal areas, is the main diagnostic technique. Further confirmation of intraocular and cerebral hemorrhages can be obtained using further imaging modalities. Ocular ultrasonography can be used to evaluate the anatomy of the eye when the hemorrhage prevents retinal vision. Terson's syndrome is characterized by hemorrhages beneath the internal limiting membrane, which can be detected by optical coherence tomography (OCT).
Despite being uncommon, fluorescein angiography may be useful in assessing retinal blood flow and detecting issues. To verify whether brain hemorrhages are present, neurological imaging is essential. In order to identify subarachnoid hemorrhage and other forms of cerebral bleeding, a CT scan is frequently the initial step. While MRA or CTA (magnetic resonance or computed tomography angiography) can be useful in identifying vascular abnormalities, such as aneurysms, that may have contributed to the hemorrhage, MRI can offer better detailed imaging of mild brain hemorrhages. An important diagnostic criterion is the temporal correlation between the cerebral hemorrhage and the commencement of ocular bleeding; because of increased intracranial pressure, the eye hemorrhage usually happens soon after the brain bleed.
Other diagnostic assessments include visual acuity tests to measure the impact on vision and lumbar puncture to confirm subarachnoid hemorrhage when imaging results are unclear. This comprehensive approach ensures that Terson’s syndrome is accurately diagnosed and managed.
Challenges in Diagnosis
editDue to its symptoms' overlap with those of other eye disorders such diabetic retinopathy, retinal vein occlusion, or hypertensive retinopathy—all of which can result in retinal or vitreous hemorrhages—diagnosing Terson's syndrome can be difficult. If the neurological history of a patient is not carefully taken into account, these similarities may result in a misdiagnosis. Furthermore, during fundoscopy, thick vitreous hemorrhage may obscure the retina, making it challenging to locate the bleeding source. To confirm the intraocular hemorrhage and prevent a delayed diagnosis, further imaging, like as ultrasound, may be required in some situations.
Intraocular hemorrhages may be mild or asymptomatic in certain patients, particularly if the bleeding is not severe. Because these people might not exhibit visual symptoms, medical professionals might simply concentrate on neurological evaluation, ignoring the necessity of an ocular examination. Furthermore, Terson's syndrome is somewhat uncommon and might not be identified right once, especially in non-specialized contexts. Delays in diagnosis and treatment may result from professionals' lack of awareness.
Assessing ocular involvement may be delayed in emergency settings involving patients who have experienced traumatic brain injuries because the focus frequently moves to stabilizing the patient's neurological status. Intraocular hemorrhage can also result from elevated intracranial pressure caused by tumors or brain swelling, but this may go unnoticed if Terson's disease is not diagnosed. In order to treat the neurological and ocular components of the illness and avoid long-term visual impairment, early detection and timely intervention are essential.
Common Misdiagnoses for Terson’s Syndrome
edit1. Diabetic Retinopathy: This condition can induce confusion, particularly in diabetic patients, by causing retinal and vitreous hemorrhages that resemble those in Terson's syndrome. Diabetic retinopathy might be the first thing considered in the absence of a complete neurological history.
2. Hypertensive Retinopathy: Because it also results in retinal hemorrhages, hypertensive retinopathy may be misdiagnosed in individuals with hypertension. This may cause a neurological bleed to go unnoticed, postponing the proper diagnosis.
3. Retinal Vein Occlusion: Especially in older people or those with cardiovascular risk factors, retinal vein occlusion, which is a blockage in the retina's veins, causes retinal hemorrhage and visual loss that resembles the symptoms of Terson's syndrome.
4. Primary Vitreous Hemorrhage: If there is no evident neurological event or other neurological symptoms at presentation, intraocular bleeding may be caused by primary vitreous hemorrhage or other isolated eye disorders.
5. Ocular Trauma: If a healthcare provider fails to take into account the likelihood that concurrent cerebral bleeding may be contributing to Terson's syndrome, intraocular hemorrhage in a patient with a history of head trauma may be mistakenly diagnosed as a direct eye injury.
Current Treatment Options and their Effectiveness. · Management of Intracranial Hemorrhage
- Surgical Intervention: Clipping or coiling to prevent re-bleeding and lower intracranial pressure.
- ICP Management: Medications or drainage to reduce pressure.
- Effectiveness: Crucial for preventing further ocular damage and stabilizing neurological function.
· Observation and Monitoring of Intraocular Hemorrhage
- Watchful Waiting: For mild cases, allowing natural blood reabsorption.
- Effectiveness: Effective in mild cases but not suitable for severe hemorrhages.
· Vitrectomy (Surgical Removal of Vitreous Hemorrhage)
- Procedure: Removal of vitreous gel and blood to improve vision.
- When Used: Recommended for persistent or dense hemorrhages.
- Effectiveness: Highly effective for vision restoration; carries some risks.
· Intravitreal Anti-VEGF Injections
- Medication: Off-label use of anti-VEGF injections to reduce inflammation.
- Effectiveness: Mixed results; beneficial for some cases, not standard.
· Laser Photocoagulation (Rarely Used)
- Procedure: Cauterizing blood vessels in cases of recurrent retinal bleeding.
- Effectiveness: Limited in Terson’s syndrome; more suited for vascular retinal diseases.
· Ocular Rehabilitation and Visual Aids
- Supportive Measures: Low-vision aids and rehabilitative services for lasting impairment.
- Effectiveness: Improves quality of life for patients with residual vision loss.
Phases of Terson’s Syndrome
edit1. Initial Onset: o A subarachnoid hemorrhage brought on by a ruptured aneurysm, or less frequently, other forms of brain hemorrhages (such intracerebral or subdural hemorrhages), is usually the origin of the abrupt increase in intracranial pressure that frequently precedes the onset of Turner's syndrome.
This rise in pressure causes intraocular hemorrhage, typically in the retina or vitreous, which causes symptoms including impaired vision, vision loss, or "floaters."
2. The Development of Symptoms:
o Depending on the size of the brain hemorrhage, neurological symptoms may include headaches, altered mental status, seizures, or unconsciousness.
o Ocular Symptoms: Severe, thick hemorrhages that drastically impair vision can occur, as well as moderate occurrences that go away on their own. In the days or weeks after the initial brain trauma, symptoms could get worse.
3. Settlement or Therapy:
o Natural Resolution: In less severe situations, the eye's blood may reabsorb itself over the course of weeks to months, progressively enhancing vision.
o Surgical Intervention: To remove the blood and restore vision, surgery (such as a vitrectomy) may be necessary if bleeding is severe or ongoing.
Recovery Potential
editVision Recovery:
Patients with mild hemorrhages often regain full or near-full vision.
Those with severe hemorrhages who undergo vitrectomy also have a strong chance of visual improvement, though outcomes depend on timely treatment.
Permanent vision loss can occur if there’s retinal damage or complications like retinal detachment.
· Neurological Recovery:
- Overall recovery is influenced by the severity of the intracranial hemorrhage and the effectiveness of treatment. Treating the underlying cause, such as aneurysm clipping or coiling, improves neurological recovery prospects.
- Neurological impairments may persist if the brain injury was severe or if complications arose, affecting long-term quality of life.
Risk of Recurrence
edit1. Intracranial Hemorrhage:Recurrence largely depends on the cause of the initial hemorrhage. For eG:
Aneurysm: Once a ruptured aneurysm is treated (through clipping or coiling), the likelihood of re-bleeding is significantly reduced.
Other Causes: Conditions like hypertension may increase the risk of future brain hemorrhages if not well-managed.
2. Intraocular Hemorrhage:
Intraocular bleeding from a single brain event generally does not recur if intracranial pressure is stabilized.
However, if there’s another instance of increased intracranial pressure, such as from a new brain bleed or re-bleeding, there is a possibility of recurrent intraocular hemorrhage.
Factors that Influence Prognosis (age, health status).
The prognosis for Terson's syndrome is influenced by several factors, including the patient's age, overall health, the severity and location of the intracranial hemorrhage, the timeliness of treatment, and the extent of intraocular hemorrhage. Younger patients generally experience better recovery outcomes due to stronger healing capacities and fewer complications. In contrast, older patients may face a higher risk of complications, such as hypertension, diabetes, and age-related changes in the brain and eyes, which can reduce their recovery potential.
Chronic health conditions like hypertension, diabetes, and cardiovascular disease increase the risk of recurrence and hinder recovery. Healthy vascular and immune systems are essential for healing and blood reabsorption; poor vascular health can lead to slower or incomplete recovery. The severity and location of the intracranial hemorrhage play a significant role in the prognosis, with severe hemorrhages and those in critical brain regions, such as the brainstem, leading to worse outcomes. Elevated intracranial pressure (ICP) exacerbates both neurological and visual complications.
Timely treatment is crucial for improving recovery. Early neurosurgical intervention and prompt ophthalmologic treatment, such as vitrectomy for severe intraocular hemorrhages, can significantly improve both neurological and visual outcomes. Access to specialized care that integrates neurology and ophthalmology expertise is also vital for optimal recovery.
Intraocular hemorrhage severity further affects prognosis. Mild hemorrhages may resolve naturally, but severe, dense hemorrhages, if left untreated, can lead to permanent vision impairment and complications such as retinal detachment. Ongoing rehabilitation and follow-up care are essential to maximize recovery, and lifestyle adjustments—such as controlling blood pressure, managing blood sugar, and avoiding smoking—can improve long-term outcomes and reduce the risk of recurrence.
Epidemiology
Terson syndrome is relatively rare, and exact prevalence and incidence rates remain uncertain due to frequent underreporting, especially in patients with severe intracranial injuries. Estimates suggest that 8-15% of patients with subarachnoid hemorrhage (SAH) develop Terson syndrome, though detection methods and study populations can cause this rate to vary. Terson syndrome (TS) is characterized by intraocular hemorrhage following an intracranial bleed, such as SAH. Reported incidence rates for TS following SAH range from 8% to as high as 46%, depending on the study and patient demographics. In one study, up to 21% of SAH patients were found to have TS. However, the true prevalence may be underestimated due to the high mortality rate linked to SAH and other brain hemorrhages, which can limit the number of patients surviving long enough to receive a diagnosis. Although TS is uncommon, it is most often associated with ruptures of the anterior communicating artery (ACommA) aneurysms.
Demographic Variations
edit- Several factors can impact both the frequency and outcomes of Terson syndrome. Terson syndrome can affect individuals of all ages, but it is more commonly observed in middle-aged and older adults, particularly those at an elevated risk for subarachnoid hemorrhage due to aneurysms. While the condition is most frequently reported in adults between the ages of 30 and 60, it can also occur in children, typically following traumatic brain injuries or less common causes like arteriovenous malformations. Pediatric cases tend to have better outcomes, owing to the faster healing capacity of younger individuals, though untreated cases can still lead to permanent visual impairments. In older adults, outcomes are generally poorer due to the prevalence of chronic conditions such as hypertension, diabetes, and cerebrovascular disease, which increase susceptibility to both intracranial and ocular hemorrhages. There is a slight male predominance in Terson syndrome, as seen in studies like one from Policlinico Gemelli in Rome, where 53% of patients were male. This may be attributed to higher rates of aneurysm rupture, which occur more frequently in men, particularly with subarachnoid hemorrhage (SAH). However, women are also affected, with factors such as hormonal changes, pregnancy-related complications, and a higher likelihood of aneurysms in certain areas of the posterior circulation playing a role. Geographically, Terson syndrome is diagnosed worldwide but is more frequently observed in regions with higher rates of subarachnoid hemorrhage, such as North America and Europe, where advanced imaging technologies like CT and MRI improve detection and management. In contrast, regions with limited healthcare resources may experience underreporting of Terson syndrome due to misdiagnosis or lack of diagnostic capabilities, particularly in settings where cerebrovascular diseases and trauma are less comprehensively managed. The scarcity of large-scale data on Terson syndrome underscores the need for further research to better understand its prevalence, risk factors, and outcomes across diverse populations.
Research Directions
Improved Early Diagnosis
edit- Research is increasingly focused on identifying reliable biomarkers or imaging techniques that could lead to earlier detection of intraocular hemorrhage in patients with intracranial hemorrhages. Given that timely diagnosis is crucial for effective intervention and visual outcomes, exploring the role of advanced imaging techniques, such as OCT (Optical Coherence Tomography) and high-definition B-scan ultrasonography, is a promising research avenue
https://www.mdpi.com/2227-9059/12/10/2336
Surgical Advances in Treatment
edit- The effectiveness of vitrectomy and the timing of the procedure continue to be key areas of study. Several studies suggest that early vitrectomy improves visual outcomes, but there is no universal consensus on the optimal timing for surgery. Research is exploring whether minimally invasive techniques and newer surgical tools can reduce complications and improve outcomes.
https://www.mdpi.com/2227-9059/12/10/2336
- Further investigation into alternative or adjunct therapies, such as intravitreal injections (anti-VEGF agents), is also ongoing to determine their role in treating retinal hemorrhages secondary to TS.
https://www.ajnr.org/ajnr-case-collections-diagnosis/terson-syndrome
3. Pathophysiology and Genetic Factors
edit- Understanding the underlying pathophysiology of TS is still evolving. Research is investigating the genetic and molecular factors that may predispose certain individuals to both intracranial and ocular hemorrhages. This could help identify at-risk populations or provide insight into why some patients recover fully while others experience permanent visual impairment.
https://www.ajnr.org/ajnr-case-collections-diagnosis/terson-syndrome
4. Long-Term Prognosis and Rehabilitation
edit- Studies focusing on long-term outcomes of TS, including visual rehabilitation and the impact of sustained visual impairment, are essential for improving quality of life for affected individuals. The role of rehabilitation services, including the use of visual aids and therapy for those with permanent vision loss, is another emerging area of research.
https://www.ajnr.org/ajnr-case-collections-diagnosis/terson-syndrome
https://www.mdpi.com/2227-9059/12/10/2336
5. Predictive Models and Risk Stratification
edit- Developing predictive models that incorporate demographic, clinical, and radiological factors to better stratify risk and guide clinical decision-making is another active area of research. These models could help clinicians anticipate outcomes and personalize treatment plans for patients with TS.
https://www.mdpi.com/2227-9059/12/10/2336
| Terson syndrome | |
|---|---|
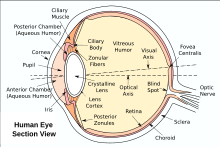 | |
| Eye anatomy(vitreous humor indicated) | |
| Specialty | Ophthalmology |
Terson syndrome or Terson's syndrome is the occurrence of a vitreous hemorrhage of the human eye in association with subarachnoid hemorrhage. Vitreous hemorrhage of the eye can also occur in association with intracranial hemorrhage and elevated intracranial pressure (ICP). Intraocular hemorrhage can be a subretinal, retinal, preretinal, subhyaloidal, or intra-vitreal hemorrhage. Its likely cause is a rapid increase in ICP.[1]
In subarachnoid hemorrhage, 13% of patients have Terson's syndrome, which is associated with more severe SAH (higher Hunt-Hess score, a marker of severity), and risk of death is significantly increased.[2]
The first known report of the association was by the German ophthalmologist Moritz Litten in 1881.[3] Still, French ophthalmologist Albert Terson's name is more commonly associated with the condition after a report by his hand from 1900.[4]
References
edit- ^ Medele RJ, Stummer W, Mueller AJ, Steiger HJ, Reulen HJ (1998). "Terson's syndrome in subarachnoid hemorrhage and severe brain injury accompanied by acutely raised intracranial pressure". J. Neurosurg. 88 (5): 851–4. doi:10.3171/jns.1998.88.5.0851. PMID 9576253.
- ^ McCarron MO, Alberts MJ, McCarron P (2004). "A systematic review of Terson's syndrome: frequency and prognosis after subarachnoid haemorrhage". J. Neurol. Neurosurg. Psychiatry. 75 (3): 491–3. doi:10.1136/jnnp.2003.016816. PMC 1738971. PMID 14966173.
- ^ Litten M (1881). "Ueber Einige vom Allgemein-Klinischen Standpunkt aus Interessante Augenveränderungen". Berl Klin Wochenschr. 18: 23–7.
- ^ Terson A (1900). "De l'hémorrhagie dans le corps vitre au cours de l'hémorrhagie cerebrale". Clin Ophthalmol. 6: 309–12.